CAUSES & CONSEQUENCES: Inside the Healthcare Crisis


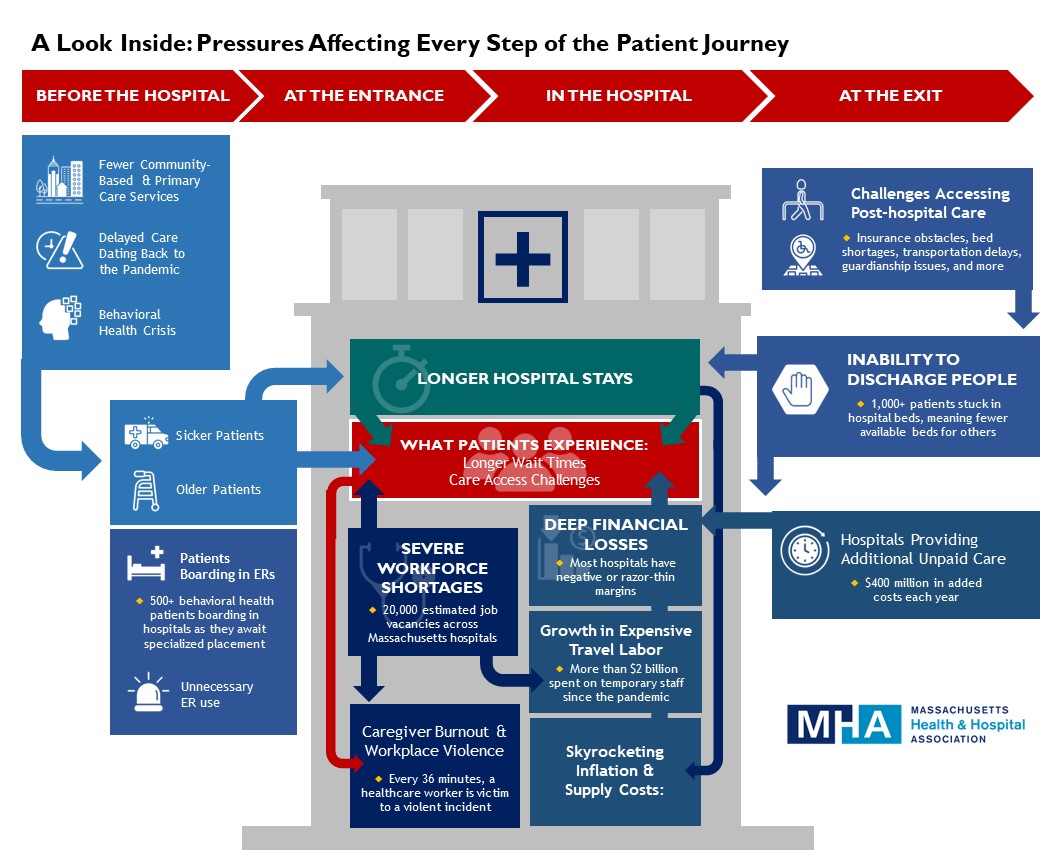
Across Massachusetts, many patients are experiencing longer wait times and other challenges as they seek the care they need. Hospitals and healthcare organizations are working tirelessly to deliver timely, high-quality care for everyone, but they are up against an unrelenting set of pressures that has made their mission more difficult than ever before.
Healthcare is in a crisis, unmatched in scope, depth, and duration.
MHA’s latest report analyzes the everyday stresses within the healthcare system, explains how they escalated so quickly, and offers solutions on what can be done to set Massachusetts on a path to recovery.
View the Report:
The word “crisis” has been used to describe many aspects of the current healthcare environment, both in Massachusetts and across the country.
- There’s a workforce crisis in which tens of thousands of positions remain unfilled across all care settings.
- A patient backup crisis is preventing 1,000 or more people from transitioning to the next level of care on any given day, leaving them stuck in hospital beds when they no longer need to be there.
- The behavioral health crisis finds upwards of 500 patients per day waiting in an emergency department or medical-surgical floor — often for days or weeks — before a specialized bed becomes available.
- Hospitals and other providers must take beds offline because they are unable to safely staff them, further fueling the patient backups and creating a capacity crisis.
- The mounting pressures have resulted in a crisis of burnout among — and violence against — healthcare workers.
- And because of all of this, many hospitals are losing money at an alarming pace, threatening their stability.
While these pressures are affecting all hospitals, patients, and communities, some segments of the population bear a higher burden than others. The COVID-19 pandemic brought greater attention to longstanding inequities in healthcare access and outcomes. Communities of color, individuals with disabilities, and people with lower incomes experience well-documented, significant differences in incidences of disease, hospitalizations, and mortality. These differences are rooted in social, political, and economic disparities and are made worse when the entire healthcare system is destabilized.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association