A CLOGGED SYSTEM: Keeping Patients Moving Through their Care Journey
Nearly one in seven medical-surgical beds is currently “tied up” as patients await discharge to other settings
A Clogged System: Keeping Patients Moving Through their Healthcare Journey shines a light on the pervasive discharge delays that are increasing hospital wait times and offers solutions to improve the flow of patients from hospitals to post-acute care settings.
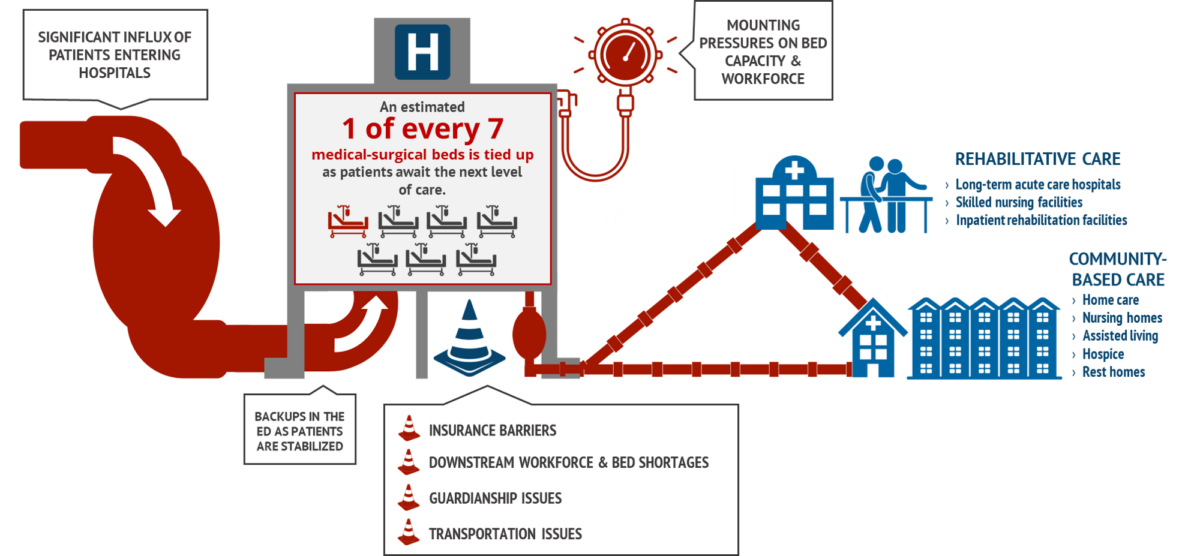
New data shows that across the commonwealth, nearly one out of every seven medical-surgical beds—15% of those in the state—are currently occupied by patients who no longer need to be in an acute care hospital. Approximately 1,200 patients are “stuck” in hospital beds as they await discharge to a post-acute care facility, a community-based setting, or a psychiatric unit.
View the Report:
The resulting backups mean patients who are awaiting post-acute care placement are not receiving the specialized treatment they need, and patients who require hospital-level care are forced to wait longer in emergency departments until the bed they need is available. This often-overlooked issue has resulted in a clogged healthcare system that causes longer hospital wait times, care access challenges, and an increasingly strained workforce.
“Even as the public health emergency has come to an end, our healthcare system is still in major distress,” said Steve Walsh, president & CEO of MHA. “This backlog of stuck patients is playing a major role in driving up wait times and obstructing access to care. We saw a tremendous level of collaboration across healthcare throughout COVID-19, and it will take that same level of focus to resolve capacity issues. MHA and our members look forward to our continued work with partners throughout the care continuum and in state government to strengthen the commonwealth’s world-class healthcare system for every patient in need of timely care.”
Improving patient transitions—whether to the home or to post-acute care facilities—is a multifaceted issue that will take a coordinated, system-wide effort to address. MHA found that the reasons for delayed discharge to post-acute care settings, as reported by hospital case managers, include the following:
- Private insurance administrative barriers
- Capacity/staffing constraints at post-acute care facilities
- Lack of guardianship/conservatorship/healthcare proxies
- Lack of secondary insurance
- Need for specialized behavioral health/substance use disorder services
- Inadequate insurer post-acute care networks
- Need for specialized medical services
- Lack of access to necessary community services
- COVID status
- Unvaccinated status
“Hospital case managers are spending endless hours and dozens of phone calls trying to get patients to the next level of care they need.,” said Amanda Ford, MSN, MBA, RN, director, Continuity of Care at Lowell General Hospital. “But the obstacles have become so numerous and so intense that it sometimes feels like an impossible task. We want to share a glimpse into this crisis and the solutions that have been identified from those of us on the front lines of patient care.”
The report includes recommendations on steps that Massachusetts can take to create a more seamless patient journey and free up acute-care beds in the months and years ahead, particularly when it comes to long-term care placements. These proposed solutions include increasing access to long-term care beds, dementia beds, and geriatric-psychiatric beds; expanding the Hospital to Home Partnership Program; and improving processes to expedite guardianship, conservatorship, and healthcare proxy cases through the courts.
“The collaboration between Massachusetts hospitals and post-acute care providers remains at an all-time high,” said Cindy Page, chief executive officer of Encompass Health Rehabilitation Hospital of Braintree, and chair of MHA’s Continuum of Care Council. “With help from state leaders, we have been working daily to improve patient transitions and to ease capacity constraints across all healthcare settings. But, as this report shows, more help is needed to address the factors that are beyond our control.”
There are several efforts already underway to address patient flow and improve hospital capacity for patients in need of post-acute care. In partnership with healthcare providers, state agency-driven initiatives include the Skilled Nursing Facility Short-Term Rehab Capacity Program, a temporary program adding short-term rehabilitation capacity to all regions of Massachusetts; and the Post-Acute Care Transitions Collaborative, which meets monthly to serve as a forum where hospitals case managers can escalate and address challenges with skilled nursing facility placements.
To learn more about the state of hospital throughput in Massachusetts and the steps that can be taken to “unclog” the healthcare system, please read, A Clogged System: Keeping Patients Moving Through their Healthcare Journey, now available at this link.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association