The Frontline of the Capacity Crisis

INSIDE THE ISSUE
> Capacity at South Shore Health
> The Assault on 340B
> Abortion Care in Mass.
> The Right Care at the Right Place
> Q & A Re: Steward
> Mary B. Conceison Award
> Transition
MONDAY REPORT
South Shore Hospital: “We Physically Have No More Space”
While nearly every hospital in Massachusetts is at or near full capacity, South Shore Hospital – located in the center of regional facility closures and service disruptions – literally does not have any more space to handle additional patients.
Every licensed, legal patient space in the hospital – hallways, converted conference rooms, single rooms converted to doubles, and more – is full.

“We physically have no more space,” said South Shore Health’s Chief Medical Officer Jason Tracy, M.D. “We’re running 550 inpatients in a 374-bed hospital.”
Due to its location in Weymouth, well south of the cluster of hospitals in Boston, South Shore Hospital has always drawn patients from a region once served by Quincy Medical Center, two hospitals in Brockton, one in Norwood, as well as Steward Health Care’s Carney Hospital in Dorchester, and the Beth Israel Leahy Health hospitals in Milton and Plymouth.
But in 2020, the last vestige of Quincy Medical Center – its emergency department – closed, followed by the flooding and closure of Steward Health Care’s Norwood Hospital, the February 2023 fire at Signature Brockton Hospital that has yet to reopen, and the abrupt closure of the large Compass Medical group in May 2023. Each of those events resulted in patients, and ambulances, streaming to South Shore Hospital. And then the Steward Health Care disruption occurred at the end of 2023, which resulted in patients moving away from Steward’s Good Samaritan Hospital in Brockton, as well as Carney, and towards South Shore Hospital. (Good Sam itself had provided important relief when Signature Brockton closed.)
The Numbers Behind the Issue
“After the Signature Brockton fire, we very rapidly saw about a 15% increase in emergency room visits, and then it stabilized over the summer,” said South Shore Health’s President & CEO Dr. Allen Smith, who has led the system since November 2020. “But when the latest news started to come out about Steward last summer, then even more patients from the Brockton region – who were probably Good Sam patients – started coming to us. And then the Steward bankruptcy news added to it even more.”
Tracy said that since the Signature Brockton Hospital closure, South Shore Hospital’s emergency department volume has increased 27%. Now 365 patients per day are coming through its ED, whereas pre-pandemic the number was about 275. Each successive hospital closure since Quincy Medical Center has led to more ED visits at South Shore Hospital. And the more patients that visit the ED, means the hospital is admitting more patients – a 38% increase in medical/surgical inpatients since Brockton Hospital closed, according to Tracy.
After the Brockton Hospital fire, Smith’s team projected the fallout and immediately hired 80 additional traveler nurses, at great expense, to handle the expected influx of patients.
“We were committed to three things,” Smith said. “First, that every patient from the Brockton region would feel welcome here and that from a social and cultural standpoint we would meet those needs. Two, we knew we had to invest in quality and make ourselves an even higher-quality institution. And third, we were going to make sure that we were protecting our employees and that entailed having reasonable staffing to handle the additional patients.” Smith said that in addition to the cost for travelers, South Shore expended many dollars on overtime and incentive pay.
Addressing the Crisis
A few initiatives underway at South Shore Hospital have helped address the capacity crisis. First, Smith said, is keeping a focus on the facility’s length-of-stay innovations that pre-dated the crisis. Teams within the hospital coordinate very closely in moving patients through the care process. A simple step of arranging for transfers to a post-acute early in a patient’s recovery process, instead of waiting to the last moment, shaves tenths of a day off length of stay, which translates into open beds.
Tracy highlighted the health system’s investment in Mobile Integrated Health (MIH) and hospital-at-home programs. MIH is for patients who require same-day urgent visits for triage and limited treatment; those patients – 15,000 over the past four years – are visited at home by South Shore Health paramedics. The South Shore Health Hospital at Home program, which started at the beginning of June, is for patients who require inpatient-level hospital care and are stable enough to receive it in their homes. Many hospitals across the state have undertaken, or are about to start, MIH and at-home programs and the innovations are, as Smith says, “exciting” as to what can be accomplished outside of a hospital’s walls.
But in the case of South Shore Hospital, neither of those innovations, or the state’s recent flexibilities regarding urgent care (see related story), are enough to fully alleviate the current capacity problem.
“Every initiative and program helps,” says Smith. “But the ideal for us is that Signature Brockton re-opens as soon as possible and Good Sam remains open. Even those openings are not a complete panacea, but they allow us to be even more efficient with our length-of-stay work, and it allows us to invest more in behavioral health to help solve that problem. It allows us to do a lot of things.”
The Concerted Effort to Hobble 340B is Harming Hospitals
The profitable pharmaceutical industry’s assault on the 340B drug pricing program is causing concern among providers that rely heavily on the program to help fund their operations.
340B empowers eligible hospitals to purchase certain outpatient drugs through wholesalers at a discounted price. This is especially critical at a time when pharmaceutical prices are growing rapidly and many patients have challenges affording the medication they need. The Center for Health Information and Analysis’s (CHIA’s) most recent cost trends report showed that aside from one-time COVID-19 payments, pharmacy costs were the largest contributor to the increase in the state’s Total Health Care Expenditures. CHIA says pharmacy spending “has consistently represented a major driver of total healthcare cost growth.”
By receiving discounts on expensive drugs from profitable pharmaceutical companies, hospitals can devote more resources to specific populations and communities, which improves access and advances health equity. Many community health programs are made possible through 340B savings, including those offering free vaccines, behavioral health and telehealth services, and free or discounted medications.
Lately, though, pharmaceutical companies have disrupted the program. The drug manufacturers won an important court case in May which found that the government overstepped its authority when it required the drug companies to provide 340B discounts to not only in-house hospital pharmacies, but also to retail pharmacies with which providers contracted. And some manufacturers are refusing to provide access to 340B drug pricing until the hospital meets what the provider community believes are unlawful demands to provide patient claims data.
“These mounting, pharmaceutical industry restrictions are diminishing savings owed to 340B hospitals, while increasing profit margins for drug manufacturers,” said MHA’s Executive Vice President & General Counsel Mike Sroczynski. “And they are being imposed at the worst possible time, as hospitals continue to struggle financially and face hardships with workforce shortages and increased medical supply and medication costs.”
State, and MHA, Focus on Climate
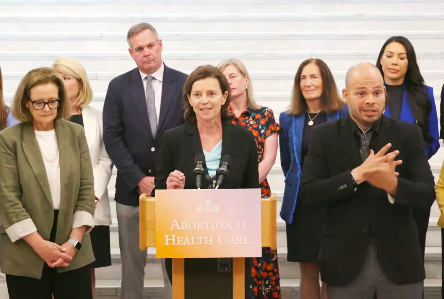
Governor Maura Healey last Monday – the second anniversary of the Dobbs decision that overturned Roe v. Wade – issued Executive Order 633, which reaffirmed and clarified state law requirements that hospitals provide emergency medical treatment, including abortion services, to patients.
Healey’s order, as well as concurrent guidance from the Department of Public Health and Division of Insurance reiterating existing Massachusetts law permitting access to abortion services, came as the U.S. Supreme Court was poised to decide a case from Idaho involving abortion. That case focused on whether Idaho’s abortion ban conflicted with the federal EMTALA law that requires hospitals to take whatever treatment necessary to stabilize a patient. Last Thursday, the court decided to dismiss that case – or not take it up – which means that a lower court ruling allowing emergency abortions at Idaho hospitals will stand while the case winds through the courts.
Last Monday, Healey’s Order 633 noted: “pregnancy termination is necessary to avoid the risk of loss of life of a pregnant person or serious harm to their health in a number of medical emergencies; … almost twenty percent of pregnancies in the United States involve a visit to the emergency department, and there is a wide range of medical conditions that might require emergency abortion care to prevent risk of infection, sepsis, hemorrhage, loss of fertility, or death.”
MHA was invited to speak at the event on Monday. MHA’s Executive Vice President and Chief Innovation Officer Valerie Fleishman thanked the governor for her leadership on the issue and said, on behalf of hospitals, health systems, and providers, “To the women and birthing people of Massachusetts, we are here for you today and every day. And we will not stop fighting on your behalf to not just preserve – but to expand – the safe and accessible reproductive care you deserve.”
State Capacity Plan Focuses on Urgent Care
The Healey Administration sent a memorandum to hospitals, health insurers, and urgent care centers last Wednesday, outlining new commercial insurance and MassHealth guidance that should help drive patients in eastern Massachusetts to urgent care centers and away from overcrowded hospital emergency departments when warranted.
As has been well reported, hospitals are at or above capacity, especially in the eastern part of the state, and the condition is worsening as uncertainty increases over the fate of the eight Steward Health Care hospitals.
Under the new commercial health insurance guidance that MHA and the insurer and urgent care associations worked out with state regulators, insurance companies will reimburse urgent care centers in eastern Massachusetts regardless of whether the urgent care center is in or out of network.
So, if an urgent care center participates with the insurer but is not in the member’s specific health plan, the insurer will reimburse the provider at the insurer’s in-network rate for the services provided.
If the urgent care center is not in the insurer’s network, the provider will be reimbursed at 135% of what Medicare would pay for those services in the provider’s geographic region.
For the 90-day period, the urgent care centers agree not to balance bill all patients, including those who are out of network and those enrolled in MassHealth. That means if a provider’s charge is $100 and the allowed amount is $70, the provider will not bill the patient for the remaining $30. Patients may still have to pay co-pays or deductibles, and an urgent care center’s policies for treating uninsured individuals is not affected.
MassHealth released a separate guidance requiring all the plans under its purview to cover services provided by out-of-network urgent care clinics. The various MassHealth plans are encouraged to clearly notify their provider networks of the expanded access, update their websites, and to “contract with additional providers that may deliver urgent care services” in eastern Massachusetts.
The guidance is effective from July 3 through October 1, 2024, in the following counties: Essex, Middlesex, Suffolk, Norfolk, Bristol, Plymouth, Barnstable, Dukes, and Nantucket.
The memo also notes, “To support this effort, the Department of Public Health, insurers, hospitals, and urgent care providers will ramp up their patient education efforts regarding appropriate use of EDs and urgent care centers.”
MHA previously created the “Right Care, Right Place” website that helps people understand when to seek care at a primary care provider, urgent care center, or emergency room. The basic message is that patients should not think twice about visiting an emergency room if they feel they need immediate, serious care. But if they are experiencing a less serious medical situation, other options may be better suited for them. MHA members as well as any healthcare organization or partner can use a series of graphics MHA created to help inform the public about where to seek care.
Many Questions, Some Answers About the Steward Bankruptcy
MHA held one of its best attended webinars in its history last Wednesday, as more than 800 people signed in to hear a 45-minute update on the Steward Health Care bankruptcy case.
Eric Gold and Schuyler Carroll, partners at Manatt, Phelps & Phillips law firm, led the webinar, which was moderated by MHA’s Executive V.P. and General Counsel Mike Sroczynski. (Gold was previously chief of the Health Care Division at the Massachusetts Attorney General’s Office.) During the 50-minute webinar, the Manatt lawyers gave an overview of the regulatory and bankruptcy process and took written questions.
What follows are just some highlights of the packed presentation:
- Bids on Steward’s eight hospitals are due July 15. If there is more than one bidder on a facility, then an auction between bidders will be held July 18. Anyone objecting to the winning bidder has until July 29 to inform the bankruptcy court. And the court will hold a hearing on the final sale July 31.
- The court decision is not the final action. State and federal regulators still have a say on whether the sale is anticompetitive, or if it is not in the best interest of patients. After the bankruptcy court accepts the winning bid, and while the regulators review that bid, the winning bidder could sign a transition services agreement to smooth the ensuing process.
- A potential negative scenario is that a winning bidder gets court approval, and then the deal is squashed by, say, the U.S. Department of Justice because of antitrust concerns. The lawyers opined that some interested buyers most likely have already reached out to the regulators to help allay those antitrust/regulatory concerns and move the process along.
- The court will take all money from sales of Steward hospitals, put it in a “bankruptcy estate,” and pay creditors out of that pool. Some creditors, such as Medical Properties Trust (MPT), which owns the hospital property and has lease agreements with Steward on them, has argued that it has priority among the creditors.
- The bankruptcy court has allowed potential buyers to negotiate directly with MPT and any unions at the hospital. A buyer could accept an existing contract a Steward hospital has with a health insurer or reject it in favor of a contract it already has with that insurer. In that case, the insurer whose existing contract has been rejected can file a claim to recover any losses. That claim would be added to the pile of claims that is building. Anyone who believes they are owed money by Steward or by the bankruptcy process must file by August 19, 2024.
- Can the Mass. Attorney General stop a sale of a Steward hospital? No, but the AG can file suit to have the court stop it.
- Can creditors sue the management of Steward to recover money? Yes.
Obviously, the bankruptcy, hospital sale, regulatory labyrinth, patient safety, and workforce concerns are substantial and complex. But the MHA webinar last week gave a good synopsis of some key points. More details to follow.
Noga Presented ONL’s Mary B. Conceison Award

Congratulations to MHA’s Vice President of Clinical Affairs, Patricia “Pat” Noga, PhD, R.N., who has been awarded the Mary B. Conceison Award for Excellence in Nursing Leadership from the Organization of Nurse Leaders (ONL).
The Conceison Award recognizes outstanding nursing service administrators who advocate for the promotion of nursing as a profession. Conceison was director of professional relations at MHA for 12 years before her death in 1981. She was known for her advocacy in promoting nursing and was instrumental in the creation of the Mass. Organization of Nurse Executives that later became ONL.
Noga oversees all of the association’s clinical activity. From her leadership role in the Caring for the Caregiver initiative, and her work in promoting worker wellbeing and anti workforce violence efforts, Noga is a staunch supporter of the healthcare workforce, and especially nurses. She previously served on the American Organization for Nursing Leadership Board of Directors, and is Adjunct Associate Professor in the Department of Nursing in the College of Nursing and Health Sciences at UMass Boston.
Nadia Raymond, PhD, R.N., regional nursing director at Brigham and Women’s Hospital, received ONL’s Karen Kirby Award for Innovation in Nursing Leadership.
Transition
Kevin Beagan has been named Acting Commissioner of the Massachusetts Division of Insurance (DOI), effective June 10. Beagan has been deputy commissioner at DOI since 2004. He takes the place of former Commissioner Gary Anderson who on May 1 became CEO of the National Association of Insurance Commissioners.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association