Telehealth Reimbursement; Building the Workforce

INSIDE THE ISSUE
> BCBSMA Understands Telehealth
> BH Roadmap’s New Toolkit
> DPH: Use Expedited Credentialing
> FOCUS ON WORKFORCE: Southcoast
> Practicing Before NCLEX
> Joseph “Jody” White
> Transitions
MONDAY REPORT
Blue Cross’ Forward Thinking Telehealth Policy
Blue Cross Blue Shield of Massachusetts (BCBSMA) has taken a dramatic step that recognizes how telehealth has transformed healthcare delivery; the state’s largest insurer announced that it will reimburse for telehealth primary care and chronic condition care at the same rates as it would if the care were provided in-person.
“We applaud Blue Cross Blue Shield of Massachusetts and are appreciative that they took the forward-thinking step of leveraging the proven benefits of virtual care,” said Steve Walsh, MHA’s president & CEO. “Care is constantly evolving and the introduction of telehealth into the equation is merely another innovation designed to improve access, make follow-ups easier, and allow patients to quickly stay in touch with those keeping them healthy. Blue Cross understands the transformational promise of telehealth.”
Since the pandemic began in early 2020, providers have seen a dramatic increase in patients seeking care through telehealth. Individuals contacting their physician or other caregiver by phone or videoconference can easily access care, avoiding taking time off from work or school for an in-person visit, and reducing their transportation costs or daycare scheduling difficulties. Telehealth also provides greater access to primary care and can reduce more expensive emergency department visits.
While the venue for care may have changed through telehealth, the provision of that care – the discussions between patient and provider, the subsequent scheduling of tests and other follow up care – has not changed. And the costs of that care still exist, from a caregiver’s hours, to paying for support staff, rent, claims submission, maintaining patient records, and more. In fact, providers have invested in telehealth, shouldering the initial costs of adopting the new technology.
As the Health Policy Commission (HPC) noted in a January report, “No providers reported that telehealth had reduced their total operating expenses.” The HPC said providers face “additional expenses for establishing telehealth technology infrastructure and continued need for physical space, administrative staff, and clinician time to schedule and perform a telehealth visit as well as in-person visits.” The HPC report recommended that reimbursement parity for primary care and chronic disease management continue for at least two more years, allowing providers to continue improving their telehealth platforms and workflow, and to develop efficient hybrid care models. The HPC found that telehealth use was highest for patients with chronic conditions.
Other Plans Threaten Cuts
BCBSMA last year had considered reducing primary care and chronic disease telehealth reimbursements by 20%. Its decision this month, after further analysis, to rescind that proposed payment cut came as a welcome relief to providers. However, unlike BCBSMA, Point32Health, the parent of Harvard Pilgrim and Tufts health plans, still plans to implement a 20% telehealth cut beginning this Wednesday, March 1. Other health insurance companies may be considering or have already reduced reimbursement.
“The Massachusetts Medical Society is incredibly pleased by this BCBSMA outcome and will continue to urge all other carriers in the commonwealth to follow their lead in recognizing that disrupting the efficacy, efficiency, and momentum of telehealth threatens patient health and the attainment of equitable access to healthcare,” Massachusetts Medical Society President Dr. Ted Calianos said. “We are grateful to BCBSMA for the opportunity to represent the physician and patient voices during critical discussions about telehealth and to our likeminded colleagues from MHA and the tMED Coalition for their partnership in advocacy.”
Most telehealth is delivered through a hybrid model. That is, a practice or hospital still maintains offices, still employs staff, and still has overhead, but merely provides some of its care via telehealth. A practice may save some money by using telehealth (latex gloves and exam room table coverings aren’t needed, for example) but the overall costs of telehealth versus in-person care are on par with each other. And telehealth appears here to stay; a Massachusetts Health Quality Partners’ survey at the end of 2022 found that 81% of patients and 75% of clinicians responding believed that telehealth will be “Extremely Important” or “Very Important” to the future of care.
Free Toolkit Available to Spread Word About Help Line, CBHCs
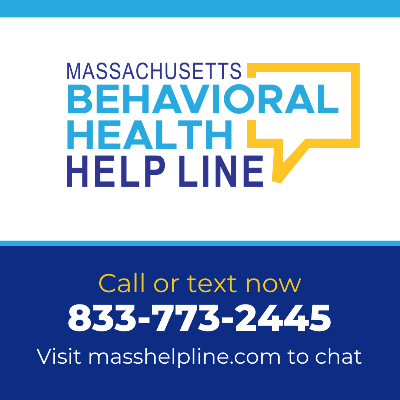
The state’s Roadmap for Behavioral Health Reform – the initiative to expand access to mental health and substance use services – has a new toolkit that providers can use to inform people about the Roadmap’s 24/7 help line, and the availability of services at 25 Community Behavioral Health Centers (CBHCs) across the state.
The behavioral health help line (by phone at 833-773-2445; or by chat at masshelpline.com/chat) is staffed by qualified professionals for mental health assessments, crisis services, substance use treatment, referrals, and more. Help line staff remain on the line until callers are connected to their next step.
The CBHCs offer 24/7 mobile crisis services for anyone experiencing a potential behavioral health crisis, regardless of insurance or ability to pay. CBHCs also provide a wide range of outpatient services, including individual and group therapy, recovery coaching, and prescribing for mental health and addiction treatment medication. Outpatient services are covered by MassHealth and some commercial insurers.
The state has released a toolkit with pre-made marketing materials to help spread the word about the help line and Community Behavioral Health Centers. There are posters, brochures, and palm cards in 14 languages available free of charge, for distribution in waiting rooms or other patient-facing areas. Here is the order form for the materials.
State to Hospitals: Use Available Expedited Credentialing
If a caregiver is credentialed at one hospital – that is, if the person has been vetted to ensure that he or she has the education, skills, and competency to practice – then another hospital can put that person to work immediately without first going through its own drawn-out credentialing process, according to a reminder that the Department of Public Health sent last week.
The reminder from the state is especially timely as hospitals across the state, but especially in Southeastern Massachusetts, step forward to assist following the fire at Signature Brockton Hospital.
The federal Centers for Medicare & Medicaid Services allowed such “expedited credentialing” during the height of the pandemic. That flexibility still exists and may be helpful to hospitals “in light of the continued strain on hospital capacity,” DPH noted in its recent e-mail.
“Such expedited credentialing should include procedures to permit a licensed independent practitioner to practice before full medical staff/governing body review as long as the licensed independent practitioner is currently credentialed at another facility,” DPH wrote. “DPH expects that healthcare facilities will not require a licensed independent practitioner that currently works at another healthcare facility in Massachusetts to collect and provide a credentialing packet prior to transferring. Instead, all healthcare facilities must rely upon the confirmation from a healthcare facility where the independent licensed practitioner is currently credentialed.”
DPH added that a hospital should make its expedited credentialing decision within one day of receiving a request from a licensed independent practitioner seeking to practice at the facility.
FOCUS ON WORKFORCE:
Bringing Joy to People’s Jobs Helps Southcoast Health Recruit & Retain

Southcoast Health has focused on the “whole-person, wellbeing” approach to help retain employees at the system’s three hospitals – Charlton Memorial in Fall River, St. Luke’s in New Bedford, and Tobey in Wareham – and more than 55 service locations across the South Coast of Massachusetts and Rhode Island.
A major component of the system’s wellbeing work is making the personal connection with workers through listening about their concerns, or stress points the workers are encountering, and what they are thinking.
The system launched a wellbeing program in 2006 and it became even more important during COVID-19 when certain daily touchpoints that workers had with each other evaporated. Cafeterias were closed due to infection concerns; staff shortages and distancing guidelines interrupted collegial gatherings. The focus now is to bring joy to people’s jobs, Southcoast says.
Learn more about Southcoast’s program, as well as about other workforce initiatives throughout the state, by visiting MHA’s Workforce Toolkit.
Allowing Nursing Grads to Practice Pre-NCLEX
One way to address the workforce shortage afflicting the state’s healthcare system is to make it easier for students who have been graduated from a nursing program, or who are in the last semester of a program, to begin working immediately at a hospital or other healthcare facility before they take their NCLEX exams – or to allow them to begin working after they take the exam but before the results are issued.
NCLEX, or the National Council Licensure Examination, is a computer adaptive test that nursing graduates must pass to be licensed in the U.S. and Canada. The problem with NCLEX is that it often takes a month or more for a graduate nursing student to get an appointment to take it, and it often takes additional months for the results to clear.
Currently in Massachusetts, registered and practical nurse graduates and students in their last semester can indeed begin to practice under the direct supervision of a licensed practitioner before taking NCLEX. That’s due to flexibilities put into place during the pandemic. Now, MHA is seeking to codify that allowance – that is, write the flexibility into law as opposed to having the flexibility in a regulation that will expire along with other pandemic-era rules.
A bill pending this session, HD1444, An Act to Improve Healthcare Workforce Development Through Graduate Nursing Practice, would allow the graduate nurses and final-semester nurse the ability to practice under direct supervision. Getting the nurses immediate bedside practice has the added benefit of helping them prepare for the NCLEX.
Jody White to Retire from Lowell General

Joseph “Jody” White, the CEO of Lowell General Hospital, announced last week that he will retire, effective September 2023. An influential figure in Massachusetts healthcare, White joined Lowell General as executive vice president and chief operating officer in 2003, was named president in 2013, and CEO of Circle Health and Lowell General in 2017.
Throughout his career, White focused on attempting to drive down the cost of healthcare while still maintaining high quality. He was an advocate for breaking down silos, embracing collaboration with physician partners, and pursuing innovation, all in the pursuit of healthcare value.
White served as chair of MHA’s Board of Trustees from June 2019 through January 2021 and was instrumental in coordinating the entire Massachusetts hospital community’s response to COVID-19. He led weekly calls between the Board’s Executive Committee and state officials and chaired weekly calls with 72 hospital CEOs that resulted in all aspects of the healthcare system working together to confront the greatest public health crisis in more than a century.
“Jody has been a powerful voice for every provider and patient throughout the commonwealth,” said MHA President & CEO Steve Walsh, who spoke with White each night during the pandemic to review the next day’s strategy. “Even in the midst of a pandemic, he demonstrated tremendous focus and selflessness on behalf of our healthcare system at-large. He ensured that the choreography between acute and post-acute providers, state and federal leaders, and many other interests was precise and able to meet the profound challenges we all faced. Most importantly, his leadership helped keep our healthcare organizations open and accessible to their communities.”
Transitions
Kate Walsh, who led Boston Medical Center for the past 13 years, will be sworn in this Wednesday, March 1 as the Secretary of the Executive Office of Health & Human Services.
Richard Burke, the president & CEO of Fallon Health since 2015, announced last week that he will retire at the end of 2023. He has been employed at Fallon for 25 years.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association