Stroke Care, Prior Auths, HPC, and more …

INSIDE THE ISSUE
> Prior Authorizations
> Mass.: We’re #1
> Stroke Care Bill
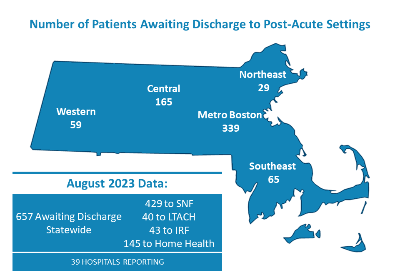
> Patients Awaiting Transfer
> HPC’s Cost Trends Report
> BHS Code of Conduct
> Schuster to Receive MHC Honor
> COVID-19 Vaccine
> Dana-Farber & BIDMC Cancer Hospital
MONDAY REPORT
A Unified Call for Prior Authorization Reform
Those testifying in favor of An Act Relative to Reducing Administrative Burden before the Joint Committee on Financial Services last Tuesday were unified on one key point – namely, they were not trying to eliminate the health insurance industry’s prior authorizations (PA), but just trying to reform them.
The bill, sponsored by Senator Cindy Friedman (D-Arlington) and former state Representative Dr. Jon Santiago (D-Boston) would require insurers to respond faster to prior authorization requests; prohibit PAs for services, medications, and treatments that have historically low denial rates; and require a PA to be valid for the duration of treatment instead of having to come back every three months to get reapproved, among many other practical, time-and cost-saving measures.

Testifying on prior authorizations (l. to r.) Leda Anderson from MMS, MHA’s Karen Granoff, and Health Care For All’s Director, Policy & Government Relations Ashley Blackburn.
“Prior auth is a tool that started as a means for insurers to control spending on costly or novel treatments, but over time it has expanded to apply so broadly and variably across plans that the burdens associated with prior auth today far outweigh the supposed benefits,” said Leda Anderson, director of Advocacy & Government Relations for the Massachusetts Medical Society. “I want to very clear about one thing: this bill does not eliminate prior authorizations. It strikes a carefully constructed balance that maintains PA as utilization management tool, but institutes smart, data-informed reforms to improve efficiency and most importantly eliminate delays and disruptions in access to care for patients.”
MHA’s Senior Director of Managed Care Karen Granoff told the committee of two challenges that hospital staff regularly encounter that are addressed in the bill. “First, hospitals operate in a 24/7 environment; insurance companies do not, meaning that it’s not unusual for a case manager to wait until the next business day for a response from an insurer on an urgent request to transfer a patient. MHA’s monthly throughput report [see story below] clearly shows that insurance issues were the number one problem in timely discharges from acute care to post-acute settings.”
Granoff said hospital personnel are often aggrieved by the fact that “clinical reviews by insurers are often undertaken by physicians who do not practice in the same/similar specialty and who have little or no knowledge about the type of treatment being requested, leading to inappropriate denials.”
“We regularly hear from HelpLine callers who have experienced a break in treatment or long wait times for critical medical services due to prior authorization. These disruptions are particularly harmful for people of color and underserved populations who are more likely to have chronic conditions,” Health Care For All Executive Director Amy Rosenthal said in a joint press release with MHA and MMS.
The Joint Committee also heard from working physicians and patients whose health status has been negatively affected by unnecessary prior authorization measures.
Recently, Cigna and United Healthcare announced the reduction of prior auth requirements by 20 – 25%. Both of these examples from national carriers illustrate that reductions in the prior authorization burdens are both necessary and feasible without entirely eliminating the practice.
The Health Policy Commission in its 2023 Health Care Cost Trends Report (see story below) recommended reform of the prior authorization process as a way to drive down healthcare costs in the state.
Getting the Most for Your Money
As state regulators, providers, insurers, patient advocates, employers, and others take a needed look at healthcare costs in the commonwealth, one question that naturally arises is: “What are we getting for the money we put into the system?”
A recent study out of Boston University provides one answer that other recent studies have confirmed: We get the best healthcare system in the United States.
Boston University School of Public Health teamed up with Sharecare, a digital health company, to produce the annual Community Well-Being Index, which found that Massachusetts is the healthiest state in the U.S. for the third consecutive year.
In June, the national Commonwealth Fund released is 2023 Scorecard on State Health System Performance, which found that Massachusetts ranked highest in the country based on 58 measures of healthcare access, quality, use of services, costs, health disparities, reproductive care and women’s health, and health outcomes. In addition to the number one overall ranking, Massachusetts was also recognized as the best state for access and affordability, reproductive and women’s health, prevention and treatment, healthy lives, and racial and ethnic equity.
And as vaccination season begins again, what state leads the U.S. in vaccination rates? That would be the Commonwealth of Massachusetts, according to a survey from Wallethub, using data from U.S. Census Bureau, Centers for Disease Control and Prevention, Health Resources and Services Administration, IBTimes, Kaiser Family Foundation and ProCon.org.
Stroke Bill Gets Hearing this Week
The Joint Committee on Public Health holds a hearing this Wednesday on a number of bills of interest to the healthcare community, including an MHA priority bill, H.2220/S.1342, An Act to Develop a Coordinated Stroke Care System, sponsored by Rep. John Lawn (D-Watertown) and Sen. Brendan Crighton (D-Lynn).
The bill would put into place many of the recommendations made by a Department of Public Health Stroke Systems of Care Work Group in 2019, which included upgrading the field assessment tool that emergency medical service (EMS) personnel use to assess stroke patients prior to arriving at a hospital; implementing additional EMS field training on identifying patient stroke acuity; improving data collection and communication between ambulance providers and destination hospitals; and creating comprehensive public education campaign about stroke symptoms and the need to seek help quickly. Then, EMS point of entry protocols could be updated to allow for EMS to bypass the closest emergency department and transport acute patients directly to a comprehensive stroke center.
However, in the FY2024 state budget passed this summer, a provision was included that requires DPH to “tier” hospitals based on stroke treatment capability and requires DPH to issue pre-hospital protocols for patients to be directly transported to comprehensive stroke centers – even over state lines – bypassing any closer community hospitals. There are only a handful of such comprehensive stroke centers in the commonwealth. The language, which is several decades old, does not include any of the other 2019 DPH recommendations to ensure proper assessment on stroke severity.
Currently, nearly every hospital in Massachusetts possesses a Primary Stroke Services (PSS) designation, meaning the facility can provide emergency diagnostic and therapeutic services 24 hours-a-day, seven days-a-week to patients presenting with symptoms of stroke. Patients with large vessel occlusions – that is, more serious strokes that occur in an estimated 25-45% of patients – benefit greatly from facilities that can provide the advanced endovascular thrombectomy (EVT) treatment. But EVT treatment is usually only available at large academic medical centers and not all of these hospitals have the necessary staff to offer the treatment on a 24/7 basis. Currently, potential stroke patients that call 911 are transported through a “spoke-and-hub” process; that is, they are brought to the nearest PSS hospital and then, if needed, are transported to an advanced facility for EVT treatment. Further illustrating the need for a comprehensive public awareness campaign, DPH data from 2019 showed that only 51% of stroke patients arrive in a hospital by way of EMS. Additionally, the data indicated that 60% of stroke patients could not identify their “last known well,” the point of time of the onset of their symptoms; or they arrived in an emergency department after 4.5 hours of experiencing symptoms. This ultimately renders them ineligible for the advanced neurosurgical treatment, as it must be administered within four hours of onset.
Despite the budget provision, the hospital community argues that An Act to Develop a Coordinated Stroke Care System still warrants legislative action.
“Absolutely no one is opposed to directly transporting severe stroke patients to an advanced facility,” said MHA’s V.P. of Government Advocacy & Public Policy Emily Dulong. “In fact, this legislation gives DPH the power to require such practice once strides have been made to improve the ability for EMS to determine stroke severity in the field. We simply want to first take the thoughtful steps offered through these bills, and as recommended by the 2019 expert panel, rather than imposing a hospital tiering system.”
Dulong continued, “We don’t believe such a rigid approach is feasible at a time when the healthcare system is facing overburdened emergency departments, unprecedented workforce challenges, a shortage of EMS personnel, and a lack of EMS transportation options. When considering these factors and the significant congestion on our state roadways, we are strongly concerned about potential adverse health events due to patients traveling long distances to comprehensive stroke centers that may have been able to receive appropriate treatment close to home.”
657 Patients Are Awaiting Transfer
The upcoming respiratory virus season (influenza and RSV, as well as COVID-19) is the first in four years in which the healthcare system will not have a series of pandemic-era regulatory “flexibilities” to rely on to help it deal with the influx of expected patients.
Flexibilities relating to licensing of healthcare personnel, the use of the state’s short-term rehabilitation capacity program, and even Medicare’s “three midnight rule” are ended, or will.
The ending of the flexibilities is causing concern among hospital discharge planning personnel, responsible for moving patients from acute care hospitals to post-acute providers, such as inpatient rehabilitation facilities, long-term acute care hospitals, skilled nursing facilities (SNFs), and home care services, among other settings.
MHA’s most recent “Throughput Survey Report” from August shows there were 657 patients awaiting discharge statewide – with 429 of them awaiting transfer to a SNF. Forty-eight percent of patients awaiting to be discharged to a SNF were waiting for 30 days or more. Between July and August patients awaiting discharge to a SNF increased by 12%.
When patients cannot be transferred, they occupy beds that are needed by other patients backed up in emergency departments awaiting an inpatient bed.
HPC Lays Out Cost Challenges, Proposed Solutions
The Health Policy Commission last Wednesday released its 2023 Health Care Cost Trends Report that tracks the annual growth in healthcare expenditures in the state, trends in spending, and more. The report also contains nine policy recommendations that the HPC says is needed to help rein in costs.
While the report notes that Massachusetts is renowned for high-quality healthcare it also points out that in some measures relating to cost it ranks low among the 50 states.
Among its policy recommendations, the HPC seeks greater oversight tools and the ability “to apply tougher, escalating financial penalties” for entities not meeting spending reduction targets. It seeks to limit “excessive commercial provider prices beyond reasonable benchmark amounts,” have greater oversight over pharmaceutical spending, and require greater standardization in payer processes, such as creating uniform medical necessity criteria and a uniform set of limited services appropriate for prior authorization.
Recognizing the severe healthcare workforce crisis affecting the state, the HPC says Massachusetts “should provide upfront support to alleviate the financial burden of education and training, including for advanced degrees and for the period between education and licensure for licensed roles, and should otherwise reduce barriers to entry. The Commonwealth should also consider policy changes supporting enhanced wages for under-resourced sectors. Finally, Massachusetts should join 41 other states (including most New England states) and jurisdictions across the country by adopting the Nurse Licensure Compact to facilitate permanent hires from other states.”
“Massachusetts hospitals and health systems continue to be fierce supporters of affordable healthcare and the HPC mission, and we and look forward to engaging with the commission on how we can build a stronger system for every patient in the commonwealth,” MHA President & CEO Steve Walsh said of the recent cost trends report. “We are especially eager to work with the HPC on its priorities that offer much-needed and immediate help to providers – including workforce development, health equity, and care access. Between 19,000 job openings, 1,200 patients needlessly stuck in hospitals, and unrelenting financial losses, healthcare leaders have been sounding the alarm on a crisis that – if gone unresolved – will prevent us from achieving meaningful cost goals. It remains an unfortunate reality that the caregivers who led our nation-leading COVID response are the last to recover from those efforts.”
Berkshire Health Systems Adopts Code of Conduct
Berkshire Health Systems is the latest Massachusetts hospital or health system adopting a Community Code of Conduct as part of a statewide effort to ensure facilities are safe, welcoming places for both patients and staff. The code is effective October 2, 2023.
“We expect all people (including staff, patients, volunteers, vendors, and guests) to be respectful and courteous,” BHS’s code reads. “Words or actions that are disrespectful, racist, discriminatory, hostile, or harassing are not welcome at BHS.

Examples of words or actions that will not be tolerated include violence, foul language, threatening or abusive behavior, offensive comments, refusal to see a clinician or other staff member based on personal traits (although BHS “will consider concerns about clinical assignments”), possession of firearms, and taking unauthorized photos, among other things.
While BHS, like all hospitals, will not refuse emergency treatment for any patient, it reserves the right under its Code of Conduct to ask patients who violate it to seek non-emergency care elsewhere.
“BHS is so proud to be the place that our community turns to in times of need, and we do not take this responsibility lightly,” said Darlene Rodowicz, BHS President and CEO. “Our Community Code of Conduct is an important step in ensuring our care environments across the county are safe, welcoming places. Every individual who walks through BHS’ doors should feel confident that they will receive the attention they deserve without fear of violence or disruptions to care. Our Community Code of Conduct supports the safety of our patients, people, and community – and communicates our strong belief that safety and healing go hand in hand.”
This January MHA released a report – An Untenable Situation & A Call to Protect the Workforce – showing that every 38 minutes in a Massachusetts healthcare facility, someone – most likely a clinician or employee – is either physically assaulted, endures verbal abuse, or is threatened. The MHA Board of Trustees in January endorsed the United Code of Conduct Principles that is included in the report, and which include measures to promote a safe and respectful environment, examples of what potential violations look like, proposed consequences for violations, and recommendations for maintaining the principles long-term. Since then, hospitals have across the commonwealth have built off those board-endorsed principles to create their own codes of conduct.
MHC Annual Dinner Honors Emerson’s Schuster
The Massachusetts Health Council annual awards dinner this year takes place on Wednesday, October 11 from 6 to 9 p.m. at Cyclorama in Boston. This year, MHC honors Christine Schuster, R.N., the president & CEO of Emerson Health and chair of the MHA Board of Trustees. Leaders of the Health Equity Compact will also be honored, as well as Edward Kaye, M.D., CEO and director of Stoke Therapeutics, and Ivana Magovcevic-Liebisch, president and CEO of Vigil Neuroscience. MHC’s annual gathering will feature Greater Boston’s celebrity chefs paired with high school culinary students in a “Where Culinary Meets Cause” theme. To learn more about the dinner, purchasing tickets, and sponsorship details, please visit here.
The Newest COVID-19 Vaccines
The newest COVID-19 vaccines from Moderna and Pfizer should be available in Massachusetts this week (if they have not yet arrived by press time). The Centers for Drug Control and Prevention (CDC) recommends everyone six months and older get the updated vaccine which has been reformulated to include a monovalent (single) component that corresponds to the Omicron variant XBB.1.5. CDC also says that if you have not received a COVID-19 vaccine within the past two months, you should get the updated vaccine.
Last Monday, Massachusetts Department of Public Health sent a special notice saying administration of the previous bivalent Moderna and Pfizer vaccine “must stop immediately.” That directive meant that between DPH’s September 11 order and the release of the new vaccine, no COVID-19 shots should have been administered in Massachusetts.
The Moderna and Pfizer vaccines are mRNA vaccines; the Novavax COVID-19 vaccine is a protein subunit vaccine, and its new formulation has not yet been approved by federal regulators. The Janssen (Johnson & Johnson) COVID-19 vaccine is no longer available in the U.S.
In issuing its approval for the new Moderna and Pfizer vaccine, the CDC noted that vaccination remains the best protection against COVID-19-related hospitalization and death. “Most Americans can still get a COVID-19 vaccine for free,” the CDC wrote. “For people with health insurance, most plans will cover COVID-19 vaccine at no cost to you. People who don’t have health insurance or with health plans that do not cover the cost can get a free vaccine from their local health centers; state, local, tribal, or territorial health department; and pharmacies participating in the CDC’s Bridge Access Program. Children eligible for the Vaccines for Children [VFC] program also may receive the vaccine from a provider enrolled in that program.” DPH says that providers already enrolled in VFC need not complete any additional steps to get the new vaccines. DPH also said that providers that are eligible to take part in the COVID-19 Vaccine Bridge Access Program already have received additional instructions.
Dana-Farber & Beth-Israel to Build New Cancer Hospital
Last Thursday, Dana-Farber Cancer Institute and Beth Israel Deaconess Medical Center (BIDMC) announced that they will build a free-standing cancer hospital in the Longwood medical and academic area that will operate under Dana-Farber’s license and provide adult medical oncology care.
While each organization will remain fully independent – including executive leadership, boards of trustees, and philanthropy – Dana-Farber, BIDMC, and Harvard Medical Faculty Physicians (HMFP) will be responsible for the coordinated clinical and organizational structure of the facility’s oncology care. Currently, Dana-Farber is affiliated with Brigham and Women’s Hospital – part of the Mass General Brigham System – for inpatient and surgical care. That affiliation will continue until the new hospital is built, which Dana-Farber and BIDMC said would take “several years,” pending regulatory approval.
“Beth Israel Deaconess Medical Center and the physicians of HMFP share our vision and are equally committed to ensuring a superior patient experience and advancing a collaborative focus on world-class cancer care and research that will benefit our region and the world,” said Laurie Glimcher, M.D., president and CEO of Dana-Farber.
Beth Israel Lahey Health’s President & CEO Kevin Tabb, M.D. said, “This collaboration and a dedicated, free-standing cancer hospital will be truly unique in Massachusetts. Our community needs and deserves both.”

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association