Steward Hospital Sales

INSIDE THE ISSUE
> Steward Hospital Sales
> Brockton Reopens
> Stuck Patients: The Promise of Home Care
> Rising Prior Auth Denials
MONDAY REPORT
Steward Hospitals Inch Closer to New Ownership
A federal bankruptcy hearing in Houston last Tuesday indicated major signs of progress for the sale of Steward Health Care’s beleaguered Massachusetts hospitals.
The hearing opened with news that Steward’s landlords, Medical Properties Trust and Macquarie Infrastructure Partners, had agreed to transfer the properties to their lender, Apollo Global Management. That gave Apollo the power to directly facilitate the sale of Steward’s hospital sites. Negotiations around land ownership are reportedly the central sticking point within the bidding process and the parties appeared hopeful that the new arrangement would help speed the process along. Judge Chrisopher Lopez had previously released Steward of its master lease with MPT and Macquarie, effectively freeing any potential buyers to work with the landowners to create new lease or purchase arrangements for the properties.
Steward’s lawyer also disclosed that negotiations with qualified bidders – which he described as “local, high-quality operators” – were accelerating and that purchase agreements could be finalized in a matter of days. In addition to the five Massachusetts hospitals, an agreement around the system’s national Stewardship Health physician group may also be close to completion.
Following the hearing, Massachusetts Senators Ed Markey and Elizabeth Warren called upon Apollo to work with Steward and Massachusetts interests to get the agreements done. Governor Maura Healey echoed that message on Wednesday, stating the parties “need to reach and finalize the deal,” per State House News Service. The potential buyers have not yet been publicized.
The federal judge also approved $30 million in advanced Medicaid funding from the state to help Steward’s hospitals operate through the end the month. The first $11 million tranche of those payments was planned for last week. The remaining $19 million is slated to be released around August 16 and hinges on signed purchase agreements for St. Elizabeth’s Medical Center, Good Samaritan Medical Center, Holy Family Hospital, St. Anne’s Hospital, and Morton Hospital.
Brockton Hospital Reopens Tomorrow
In a highly anticipated step for the healthcare system at-large, Signature Healthcare Brockton Hospital will re-open tomorrow, 18 months after a fire shuttered most of its care services. A 10-alarm electrical fire in February of 2023 forced the immediate closure of the facility. In the time since, the hospital has undertaken an extensive set of repairs and upgrades to make the building viable for patient care.
The Tuesday re-opening brings online a revamped emergency department that includes a new 12-unit behavioral health triage operation. Among the other upgrades are a new outpatient surgical facility and main lobby, both of which the hospital says were designed to be more convenient and welcoming for patients. Signature also secured a 1.5-megawatt solar array to offset the building’s carbon footprint and new machinery for its cardiac catheterization lab. The maternity, pediatric, and behavioral health units remain closed.
“Signature Healthcare Brockton Hospital has provided safe, quality healthcare to the community for the past 125 years, and we are dedicated to continuing this legacy for another 125 years and beyond,” said Signature Healthcare president and CEO Robert Haffey.
The announcement is especially welcome news for the southeast region, where hospital capacity constraints are among the most severe in the state. The fire at Brockton, the previous closure of Steward’s Norwood Hospital, and the overnight shutdown of Compass Medical have all resulted in increased caseloads for hospitals along the Route 24 corridor.
Leaders from Signature Healthcare recently shared their account of the crisis response and subsequent rebuilding journey in this MHA webinar. The organization created walk-in urgent care centers and moved numerous patient services to outpatient sites as part of that plan.
As Patient Backups Persist, Can SNF Care at Home Help?
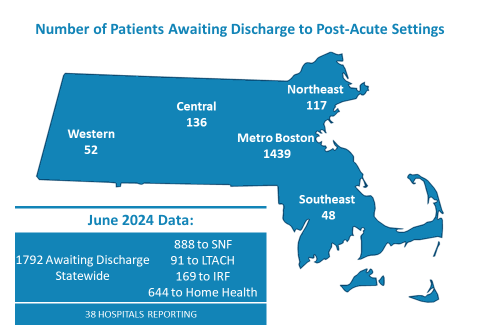
New MHA data shows that 1,792 patients were stuck in Massachusetts hospitals in June because they could not be discharged to a nursing home, rehabilitative facility, or home-based care. The association tracks this patient “throughput” issue, a growing factor behind long wait times and the statewide capacity crisis, on a monthly basis.
The June tally of stuck patients was unmoved from May’s 1,792 total. There were, however, fluctuations across the type of care patients were awaiting care. The percentage of patients in need of discharge to long-term care hospitals, inpatient rehab facilities, and home health dropped slightly. The count of patients requiring nursing home placements increased by 3%, with a third of those patients awaiting a placement in a skilled nursing facility for 30 days or more.
While the provider community advocates for reforms to ease the logjams – such as insurance improvements, cross-sector partnerships, and expedited legal remedies – state government and local hospitals are also exploring ways to improve patient flow through home-based services. Two such efforts supported by the Executive Office of Health and Human Services (EOHHS) were announced in recent weeks.
UMass Chan Medical School, through its connection with UMass Memorial Health and Baystate Health, will be studying the experience of 650 recently hospitalized individuals as those patients receive skilled nursing care at home. Researchers will measure rehospitalization rates among participants, as well as how their functional status and satisfaction compare to care delivered in traditional skilled nursing settings. EOHHS is providing $6.5 million for the research.
Mass General Brigham is undertaking a related study with 300 patients across its system. 150 participants will receive at-home rehabilitation care and the other 150 will be placed in skilled nursing settings. Similar to the UMass approach, MGB will look to compare the groups for clinical outcomes and satisfaction for patients, their caregivers, and their families. EOHHS has granted $4.6 million for the study.
“Capacity constraints at Massachusetts healthcare facilities compel us to examine every innovative tool to care for patients in a timely and convenient manner, and our hospitals are proud to be partnering with the state to explore new and highly promising care models with this goal in mind,” said Adam Delmolino, MHA’s senior director of virtual care and clinical affairs. “This is a prime opportunity to measure the success of skilled rehabilitation care in the home, assess the role it can play role in moving patients out of hospital settings, and inform the investments and regulatory framework that our commonwealth should consider to support innovative care moving forward.”
KFF Report: Unwarranted Prior Auth Denials are Rampant
The role of prior authorization – or the permission healthcare professionals must get from insurance companies before they deliver certain services – has been the subject of increased scrutiny from local and federal lawmakers. When speaking about the care delays and administrative burdens brought on by PA, Massachusetts providers and patient advocates often single out what they perceive as especially egregious practices from national Medicare Advantage (MA) plans. A new report from KFF seemingly confirms their experiences.
KFF’s review found an increase of 9 million prior authorization requests across national Medicare Advantage insurers in just a three-year period (2019 to 2022). The MA plans rejected a total of 3.4 million prior auth requests in 2022 alone. And among the denials that were appealed, a vast majority – 83% — were eventually reversed, meaning the clinician’s original judgement on the proper course of patient treatment was justified. According to local healthcare providers, patients may end up getting the services or medications they need in these cases, but only following delays that are potentially dangerous for their health, a series of administrative obstacles that drive worker burnout, and added waste to the system.
“Medicare Advantage insurers are required by law to provide the same if not more services than traditional Medicare, but they often do not,” one local case manager from a large hospital system told MHA in June. “And they’re doing a disservice to their patients by restricting them and causing long delays in getting to the next site of care.”
In Massachusetts, a third of the eligible population is enrolled in a Medicare Advantage plan. The hospital community has repeatedly expressed its support for increased federal oversight of MA plans. MHA recently signed on as a supporter for the bipartisan Improving Seniors Timely Access to Care Act, which would enshrine recently approved CMS prior authorization regulations into statute and ensure that no future administration could undo those improvements for Medicare Advantage members.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association