PLEASE NOTE: MHA has upgraded its Member Portal. Click here to gain access.
Senate Budget, Housing, Safety Net

INSIDE THE ISSUE
> Focus on Capacity
> Senate Budget
> Worries Over Safety Net
> Housing & Health
> Data Breach Notification
> Federal & State Investigations
MONDAY REPORT
Steward Situation Puts Focus on Capacity
As Steward Health Care continues its attempts to sell off its hospitals and exit Massachusetts, the system’s problems are generating a response across the commonwealth’s entire healthcare ecosystem.
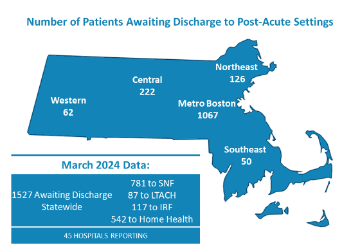
MHA’s monthly hospital throughput report that tracks how many patients are stuck in hospital beds awaiting transfer to the next level of care showed a spike in the most recent report from March. According to the MHA survey, 1,527 were patients awaiting discharge from 45 reporting hospitals. The February report showed 919 stuck patients in 41 hospitals.
While much of the month-to-month increase in the MHA report can be attributed to more, larger hospitals reporting, MHA members near Steward hospitals are reporting a steady increase in the volume of patients coming through their doors.
At a press conference last week, Governor Maura Healey and Health & Human Services Secretary Kate Walsh stressed that Steward hospitals were still open for business and that patients should still use their services.
Senate Budget Debate to Begin Next Week
The Senate Ways & Means Committee released its FY2025 state budget proposal last week – a $57.9 billion plan that, if passed as is, would provide free community college and free regional transit authority transport.
Importantly, the Senate proposed budget contains the language the House approved regarding the hospital assessment proposal that MHA and the Executive Office of Health and Human Services created and that the MHA Board of Trustees approved in April. That plan increases the tax on hospitals but ultimately results in more federal dollars flowing back to the state in federal Medicaid funding.
MHA said it supports the Senate Ways & Means’ focus on funding important behavioral health and substance use disorder programs, as well as funding the Department of Mental Health programs relating to adult support services, continuing care beds, and emergency department diversion programs, among other initiatives.
Debate on the Senate budget is expected to begin the week of May 20. Healthcare interests are also prepared for the House to take up deliberations on its healthcare reform bill – H.4620, An Act Enhancing the Market Review Process, as soon as this week.
Growing Safety Net Concerns Spurs Budget Amendment
The Health Safety Net (HSN) – the fund that is used to pay for care for those who have low incomes and are uninsured – is becoming more unstable due to a series of events.
The HSN is funded by hospitals and health insurance companies, each at $165 million per year; the state is directed to fund $30 million annually by statute, but historically only contributes $15 million. This funding always has been insufficient. If the cost of care for patients exceeds the amount of money in the HSN, hospitals are solely responsible for covering any HSN shortfall at the end of a fiscal year.
A confluence of factors is now increasing the financial instability of the program and will threaten the viability of the of the safety net. Uninsured volume has increased both at hospitals and community health centers, some of which is likely tied to MassHealth redeterminations. The state is also expected to reprocess all claims to correct for an update to the “grouper” mechanism used in that processing, which will increase the FY2023 and FY2024 shortfalls. To fund the Medicare Savings Program eligibility expansions, the state transfers funds out of the HSN at an increasing amount. The financial instability of Steward hospitals has also contributed to the HSN financing challenges.
By MHA’s estimates, the combination of factors will drive the shortfall to levels unseen in 20-plus years when uninsured costs peaked and spurred the state to enact the historic 2006 health reform law. According to MHA, the combined FY23 and FY24 health safety net shortfalls – all falling entirely on acute care hospitals – will reach $380 million in aggregate. Without further action, the FY25 funding shortfall will exceed $220 million – a total of $600 million for these three fiscal years combined. This comes at a time when hospitals already are experiencing enormous financial pressures and most are operating on negative or razor-thin margins. Last Friday, MHA filed an amendment to the Senate’s state budget proposal to address the destabilizing effect of the Health Safety Net shortfall on hospitals.
Gov. Healey, Health Leaders Discuss Intersection of Housing and Health

Boston Medical Center hosted Governor Maura Healey, Lieutenant Governor Kim Driscoll, Health & Human Services Secretary Kate Walsh, Housing and Livable Communities Secretary Ed Augustus, and healthcare leaders from across the state in a forum to discuss how housing affects public health.
Secretaries Walsh and Augustus led the discussion that focused on the challenges providers face in attracting workers due to the high cost of housing in the state, as well as how housing insecurity affects health outcomes.
“As we build solutions to our housing crunch, we’re also giving Massachusetts residents the ability to lead healthier and happier lives,” Lt. Gov. Driscoll said.
Studies have shown that people who experience chronic homelessness face worse physical and mental health outcomes, increased mortality, and higher healthcare costs. People who are housed but who face housing instability (such as moving frequently, falling behind on rent, etc.) are also more likely to experience poor health. Low-income families that have difficulty paying their rent, mortgage, or utility bills are less likely to have a usual source of medical care and more likely to postpone needed treatment. Renters who spend more than 50% of their income on rent and utilities are more likely to face difficulties purchasing food. And poor housing conditions – that is, water leaks, poor ventilation, dirty carpets, or pest infestation – have been associated with poor health outcomes, most notably those related to asthma.
The lack of affordable housing also means that hospitals and other care providers have difficulty finding the healthcare workers needed to care for those experiencing poor health outcomes due to their housing.
“Three years ago, during the COVID-19 outbreak, we were calling our healthcare workers heroes, and now those same heroes can’t afford a place to live in Massachusetts,” Secretary Augustus said. “They need our help now in making Massachusetts more affordable.
The governor used the forum to promote her administration’s $4 billion Affordable Homes Act that would devote funding for 18 separate initiatives, while creating a statewide housing plan, allow accessory dwelling units, and allow local option transfer fees, among other things. (See a fact sheet here.)
Among those lending support to the governor’s plan are the following members of MHA’s Board of Trustees: Alastair Bell, M.D., president & CEO of Boston Medical Center Health System; Anne Klibanski, M.D., president & CEO, Mass General Brigham; Lynette Watkins, M.D., president & COO, Cooley Dickinson Hospital; Michael Dandorph, president & CEO, Tufts Medicine; Michael Lauf, president & CEO, Cape Cod Healthcare; and Eric Dickson, M.D., president & CEO, UMass Memorial Health.
Said MHA President & CEO Steve Walsh, who attended last Thursday’s forum, “Affordable housing has the power to improve every aspect of Massachusetts healthcare: the vibrancy of its workforce, the stability of its communities, and the everyday wellbeing of its patients. Our hospitals and health systems are proud to partner with the Healey-Driscoll Administration on this urgent priority – including through a nation-leading commitment to screen patients for their housing needs at the point of care. This is a chance for Massachusetts to lead once again on an issue that matters to the health of its community members.”
Providers to United Health Group: You Broke It, You Fix It
Earlier this month, the CEO of United Health Group (UHG) Andrew Witty told the U.S. Senate’s Finance Committee that “maybe a third” of all Americans had their personal health information stolen in the February data breach at UHG subsidiary Change Healthcare. In an April 22 press release, UHG said it would “will provide appropriate notifications” to those affected and offered “to make notifications and undertake related administrative requirements on behalf of any provider or customer.”
Last week, the American Hospital Association and five other national provider groups wrote Witty to remind him of his company’s obligations to notify consumers whose data may have been stolen. The letter was spurred by a posting on the U.S. Health & Human Service’s Office of Civil Rights’ (OCR) website that noted “while the covered entity [UHG] is ultimately responsible for ensuring individuals are notified, the covered entity may delegate the responsibility of providing individual notices to the business associate.” The bolding in that notice is from OCR and “business associate” could refer to hospitals and health systems.
AHA and the other providers were taken aback by what seemed like an attempt to shift notification responsibilities from UHG, whose security shortcomings were responsible for the data theft, to the providers who have lost millions of dollars in revenue due to the breach.
“UHG has already correctly recognized that it—not covered entities like health systems and hospitals—is in the ‘best position’ to notify individuals of any breach,” the providers wrote. “Accordingly, we urge UHG to immediately notify OCR, state regulators, Congress, the media, and other relevant stakeholders that it is formally accepting a delegation from all covered entities to make breach notifications on their behalf.” The bolding is from AHA, et. al.
DOJ Opens New Healthcare Investigation Arm
The U.S. Department of Justice announced last week it is creating a Task Force on Healthcare Monopolies and Collusion (HCMC).
“Every year, Americans spend trillions of dollars on healthcare, money that is increasingly being gobbled up by a small number of payers, providers, and dominant intermediaries that have consolidated their way to power in communities across the country,” said Assistant Attorney General Jonathan Kanter. He said the task force will “root out monopolies and collusive practices that increase costs, decrease quality, and create single points of failure” in healthcare.
Recently, members of the state’s Congressional delegation and others have called for investigations into and regulation of the large United Health Group (UHG), and the failing Steward Health Care system. In Massachusetts, the Health Policy Commission will be reviewing the potential purchase of Steward’s physician group by UHG subsidiary OptumCare if it stays on track in the midst of the federal investigation. The HPC announced last week that its review is hung up because “the parties have still not submitted key required information and many details are still outstanding.”


 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association