Revamping the Benchmark; PHE Ends

INSIDE THE ISSUE
> Cost Growth Benchmark
> PHE Ending in Mass.
> Vaccines
> Prior Auths Rapped
> MassHealth Redetermination Webinars
> Transitions
MONDAY REPORT
2012 Benchmark Does Not Apply to 2023 – But Can Be Fixed
The Health Policy Commission, together with the Joint Committee on Health Care Financing, met last Wednesday to discuss the state’s healthcare cost growth benchmark. Conceived through the 2012 cost containment law, the benchmark, which is meant to limit total healthcare spending growth annually, is currently set at 3.6%.
Two main themes emerged from Wednesday’s hearing: first, that patients and employers continue to face rising healthcare costs and, second, the benchmark as constructed more than a decade ago is not really accounting for the dramatic changes that have occurred since then – most notably, costs related to the once-in-a-generation pandemic, the workforce shortage and rise of “traveler” workers, and the current inflationary pressures on all sectors of the economy.
“The benchmark simply wasn’t designed to measure the biggest cost drivers in today’s market,” MHA’s President & CEO Steve Walsh said in his hearing testimony. “Healthcare providers have done whatever it takes to adjust to those cost pressures and remain accessible for their patients – but those measures have come with a staggering price tag. For instance, we now know that hospitals spent more than $1.5 billion on travel labor in FY22 alone. That’s a 610% increase from pre-pandemic spending … [Temporary labor] is the single biggest cost pressure for every hospital and health system as we speak. And yet there is not a way to account for it using the current approach to the benchmark, which relies on data from two years ago.”
Walsh noted that other factors affecting healthcare cost growth in Massachusetts – factors that were not prevalent in 2012 when the benchmark was created – include rampant inflation, the effects of patients’ deferred care during the pandemic, fast-rising pharmaceutical prices, the landmark new Medicaid waiver, the behavioral health and post-acute boarding/capacity crisis, and the infrastructure improvements providers are making to enhance their cybersecurity, respond to climate change, and build more sustainable facilities.
“So, the simple truth is this: a benchmark that cannot reflect the realities of today is not a benchmark that can serve the cost needs of today,” Walsh said. “And an approach that is stuck in 2012 will only hold us back. Over the past year, this commission has taken bold steps regarding the workforce and care innovation, and it shows that you understand how to imagine the future.” Walsh implored the HPC “not to be stuck in 2012.”
The other prevalent theme emerging from last Wednesday’s hearing, from MHA and others, is a recognition that any change to solve the workforce shortages, rising pharmaceutical costs, excess insurer profits, and more must be addressed with the same “all-hands-on-deck” strategy that existed in 2012 when the benchmark was created.
“MHA and our members remain fully committed to the work of the HPC and ensuring patient access and affordability, and we are here as partners to help this benchmark tool find its footing again,” Walsh said.
State Public Health Emergency to End in May
In tandem with the previously announced end of the national COVID-19 Public Health Emergency (PHE) on May 11, the Massachusetts PHE will also end on the same day, the Healey Administration announced last Wednesday. Also effective May 11, Executive Order 595 requiring all executive branch state employees to be vaccinated against COVID-19 is rescinded.
While the administration is lifting the PHE, Governor Healey said she is filing legislation to extend some of the flexibilities that existed under it – namely, allowing staffing flexibilities for out-of-hospital dialysis centers, allowing ambulance transports to be staffed by a single EMT provider and a first responder driver (rather than two certified EMTs), and authorizing certain non-Medication Administration Program certified staff to administer some prepackaged medications in community settings.
Many other flexibilities, however, will end on May 11. These include limiting the types of healthcare professionals who can administer vaccines; increasing the supervision of physician assistants to pre-pandemic levels; and lifting the requirement that individuals within healthcare facilities must wear face masks. Such facilities, however, can set their own masking rules.
MHA recognized the imperative to end the PHE and said in a statement released to the media: “It’s important for community members to remember that while the crisis of pandemic has thankfully abated for much of our society, Massachusetts’ healthcare system remains under intense pressure. We ask everyone to continue to comply with the policies of individual healthcare facilities and to continue taking all the necessary COVID-19 precautions. We are grateful for the support of the Healey-Driscoll Administration in prioritizing the needs of providers and helping our system recover.”
Vaccines Are Still Important, but Some Cautions and Guidance
The Public Health Emergency is ending because progress has been made in protecting the public from the still-in-existence COVID-19 virus. Going forward it appears that regular vaccines against COVID will be strongly recommended, just as regular flu vaccines are needed. Last week, there were some new vaccine developments.
The Food & Drug Administration (FDA) has amended the emergency use authorization (EUA) of the Pfizer bivalent vaccine, allowing its use as a booster in children aged 6 months to 4 years at least two months after the children have completed a primary vaccination regiment of three doses of the Pfizer monovalent vaccine. If such children received two initial doses of the monovalent vaccine and their third primary dose was of the bivalent vaccine – which has been the recommendation since December 2022 – then the children are NOT eligible for the Pfizer bivalent booster; that is, they have enough protection, the FDA says. But, again, if their first three doses were of the monovalent vaccine, then they can get the booster.
Also last week, the FDA reissued the EUA for the Johnson & Johnson vaccine, but added myocarditis and pericarditis to the list of adverse conditions that could result from the vaccine. The FDA had previously warned about thrombosis with thrombocytopenia syndrome (that is, blood clots and low platelet count) relating to the J&J vaccine. In issuing the reauthorization, the FDA said the vaccine’s benefits outweigh its risks.
With the end of the PHE, the likely need for future vaccines, and the government’s move to “commercialize” vaccines, there has been much discussion about who will pay for needed vaccines going forward. The Administration for Strategic Preparedness and Response recently issued this “Commercialization of COVID-19 Medical Countermeasures” FAQ that discusses post-May 11 vaccines. People on Medicaid and Medicare, or who have insurance through the Affordable Care Act, will not pay for vaccines; those with employer-based commercial coverage, likely will not pay initially, but there could be some cost sharing.
Prior Auth: Delays Care and Adds Administrative Burden
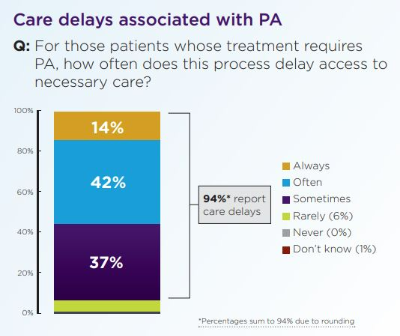
Prior authorizations – that is, getting an OK from health insurance companies for certain medical treatments – are coming under increasing fire as the federal government considers a final rule that would mandate that insurers streamline their prior auth policies.
The American Medical Association released a survey last week showing 94% of doctors attribute patient care delays to insurer prior authorizations. The doctors report that patients often abandon treatment altogether due to prior auth bureaucracy, and 33% of physicians say that prior authorizations have led to a serious adverse event for a patient in their care.
The American Hospital Association wrote a letter reminding the Centers for Medicare and Medicaid Services (CMS), which is drafting the final rule, that any prior authorization guidelines it produces will be meaningless unless there is strict enforcement and oversight from CMS.
MHA sent its own detailed letter to CMS urging prior authorization overhaul. “The health plan prior authorization process has long been recognized as a key source of administrative burden, delays in patient care, denials of medically necessary treatment, and provider frustration,” wrote MHA’s Senior Director of Managed Care Karen Granoff. “…We are therefore pleased the proposed rule includes important policies to remove inappropriate barriers to patient care by streamlining prior authorization processes for affected health plans and providers. These regulations would reduce the amount of time spent on phone calls and paperwork, expedite the health plan decision making process, and allow clinicians to spend more time focusing on patient care.”
Also weighing in was the Massachusetts Medical Society – Massachusetts Health & Hospital Association Joint Task Force on Physician Burnout, which for the past four years has influenced the conversation around unnecessary administrative burden, physician burnout, and clinician wellness. The task force urged CMS to take steps to encourage more effective automation and streamlining of the prior authorization process by requiring, among other things, an electronic prior authorization system that would be universal across all payers. “Many experts believe 40 to 60% of all prior authorizations filled out by providers are on patients who do not even require prior authorization!,” the MMS-MHA Task Force wrote. “Even automating just the first stage of the prior authorization process … could eliminate half of all prior authorizations filled out by the providers.”
MassHealth Redetermination Webinars
When the federal government declared a public health emergency in March 2020, MassHealth put protections in place that prevented members’ MassHealth coverage from ending. But with the PHE ending on May 11, these MassHealth protections are ending as well, and the state’s Medicaid program will soon return to the standard annual eligibility renewal processes. Beginning on April 1 and continuing through the year, MassHealth will review the eligibility of all members to confirm they are still eligible for their current coverage. This is a massive undertaking.
On Thursday, March 23 from 2 to 3 p.m., the Massachusetts Health Care Training Forum will hold a webinar to explain the redetermination process, identify key timelines, and more. The same content will be presented on Tuesday, March 28 from 10 to 11. Click on either link to register for one or the other.
Also on Thursday, March 23 from 3 to 4 p.m., MassHealth will hold another webinar on how the redeterminations specifically affect children and parents of children on MassHealth. All entities that work with MassHealth members – including many components of the healthcare community – are invited to attend. After registering by clicking on the date above, you will receive a confirmation e-mail containing information about joining the meeting. The session will be recorded and ASL interpretation will be provided.
MHA is also holding briefing sessions between its member working groups and Health Care For All; the state has contracted with Health Care For All to help execute a public messaging campaign – particularly in high public-payer communities.
Transitions at EOHHS
Dr. Kiame Mahaniah will join the Executive Office of Health & Human Services (EOHHS) as Undersecretary for Health, effective April 24. Dr. Mahaniah is a practicing physician in the field of addiction and primary care and has most recently served as CEO of Lynn Community Health Center. He holds a BA from Haverford College, an MBA from UMass Amherst, and a medical degree from Thomas Jefferson University.
Mary McGeown will join as Undersecretary for Human Services, effective April 10. McGeown has provided executive leadership to the Massachusetts Society for the Prevention of Cruelty to Children since 2012. She was previously deputy commissioner for the Massachusetts Department of Youth Services. She holds a BS from Boston University.
Joanne Marqusee has been appointed Assistant Secretary for Operational Effectiveness at EOHHS. Marqusee was the president & CEO of Cooley Dickinson Hospital between 2014 and 2021, and most recently was EVP/Chief Integration Officer at Tufts Medicine. She has a BA from Cornell and a Masters in Public Policy from Harvard Kennedy School.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association