Reforming Prior Authorizations

INSIDE THE ISSUE
> Throughput Issue Worsens
> The Human Side of Prior Auths
> Grants to Expand Hospital-to-Home
> Graduate Nurse Regulations
> Change Breach Notifications
> Artificial Intelligence
MONDAY REPORT
In April There Were 1,972 Patients Stuck in Mass. Hospitals
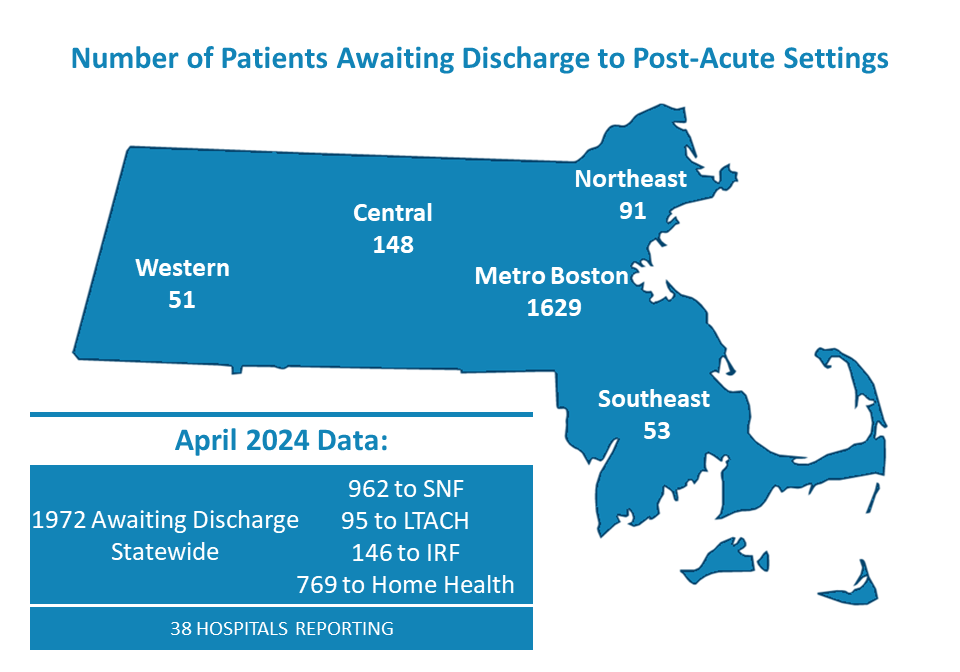
The latest MHA throughout report shows that in April there were 1,972 patients stuck in Massachusetts hospital beds awaiting transfer to the next level of care at a rehabilitation facility or home care.
The number jumped from the previous month’s total of 1,500 patients, due partly to rising patient volumes across the system but also because of new reporting from two large academic medical centers. While the new reporting was added to the report, it is important to note that the nearly 2,000 stuck patient figure is from just 38 of approximately 64 reporting hospitals in the state.
The inability of a patient to transfer to the next level of care affects not only the health and recovery of the patient, but also hospital finances and worker wellbeing (see next story).
The instability of the Steward Health Care system is contributing to the problem, as are other facility closures in recent years, including the increase in nursing home closures across Massachusetts. Even if beds were increased through pandemic-era flexibilities, it’s unclear if there would be enough healthcare workers to staff them. “Among other tools, we need Massachusetts to join the Nurse Licensure Compact (NLC) so we can simplify the licensure process for RNs to come and work in our state. And we need prior authorization reform so we can cut through the needless red tape hampering patient transfers,” said MHA’s Senior Vice President of Government Advocacy and General Counsel Mike Sroczynski. “We need meaningful healthcare legislation that reflects the realities and voices of today’s healthcare system. All of these things are within reach before the legislative session ends.”
Hospital Case Managers: Insurer Prior Authorizations a Problem
As the Massachusetts healthcare system reels from having nearly 2,000 patients stuck in Massachusetts hospitals and unable to transition to the next level of needed care (see above story), the collective focus of policymakers and the healthcare community is on how to resolve the problem.
Last week, MHA sat down with three case managers from a large hospital system to discuss the common problems they face once a patient has been assessed for discharge to some form of rehabilitative care. The case managers are clinical professionals who work with other clinicians – occupational and physical therapists, speech pathologists, and physicians, among others – as well as with skilled nursing facilities, health insurance companies, patients, and their families to orchestrate care transitions for patients. And the case managers all agree that the major problem with the process – the sand in the gears of care transitions – is the health insurance company prior authorization process, especially those from Medicare Advantage insurers.
MHA has filed legislation jointly with the Massachusetts Medical Society and Health Care For All that would address some of the difficulties patients and providers encounter from commercial health insurance companies’ prior authorization policies. The legislation would not eliminate prior auth and still allow insurers to use it as a means of controlling costs; but under the MHA-MMS-HCFA proposal, low-value prior authorization requirements would be eliminated and the process streamlined.
According to an MHA report, Massachusetts can remove as much as $1.75 billion in wasted costs through “sensible” insurance-related reforms – particularly through simplifying prior auth processes.
Delays of 5-to-10 Days
“Take, for example, the very common example of a patient who on Thursday gets assessed by the physical therapist, who recommends short-term rehab for the patient,” says one case manager. (The managers requested anonymity to avoid any further friction with the insurers with which they deal.) “One of our case managers talks to the patient’s family on Thursday and makes the referral for rehab, anticipating that the patient will be ready the next day.”
The first difficulty encountered is finding an open bed at a skilled nursing facility (SNF). But if a bed is found, the SNF will request authorization from the insurer for the transfer.
“And then we’re in a holding pattern,” the case manager says. “It takes two-to-three days for a prior authorization. And while we’re a seven-days-a-week operation, the insurers, especially the national Medicare Advantage plans, don’t work on the weekends. So now we’re into the following Tuesday to move a patient who we identified on the previous Thursday was ready to be transferred.”
The system case manager did note that interacting with Massachusetts-based insurers is generally easier than dealing with the national Medicare Advantage plans: “We can often get on the phone with a local insurer and say, ‘Please, can you move this patient to the top of the list.’”
Denials Extend the Process
A five-day transfer delay is troubling, but more disturbing is an insurer’s arbitrary denial of an authorization request, which will extend the transfer delay even longer.
“Often an insurer will say, for instance, that a patient can be managed at home even though we’ve conducted an assessment indicating that rehab is necessary,” one case manager says. “So we have to appeal it, supplying additional clinical information, or sometimes there is a peer-to-peer call between our physician and the insurer’s clinician. That means a hospital physician, who is supposed to be caring for patients, has to take time to coordinate a phone call, which often can be a laborious process to nail down a time, and often results on them being put on hold as they wait to talk to somebody.”
Appealing a denial can take days. And once the weekend comes, the process is shut down until the insurer’s utilization teams return to work on Monday morning. That means a patient can be stuck in a hospital bed for 10 days or more.
The Effect on Patients
When a patient is stuck in a hospital after being cleared for discharge, problems mount. Insurance companies typically pay hospitals a fixed amount per-patient, per-diagnosis. If a patient is stuck in a hospital for additional days after their course of care has been completed, the hospital generally does not receive any additional funding and often must absorb the additional costs on its own – to the tune of more than $400 million each year across all Massachusetts hospitals. Plus the occupied bed cannot be used to help ease overcrowding on a hospital’s emergency department.
But the main harm from the stalled prior authorization process is to the patient.
“Hospitals are not set up to provide multi-hour rehabilitation therapy to patients, so they’re deconditioning while they are waiting, which means it takes even longer for their recovery process once they do get into a rehab,” according to the case manager. And the longer a patient is forced to stay in a hospital, the greater chance he or she has of contracting a nosocomial infection.
Patients stuck in a hospital, aware of the prior authorization problem, may naturally try to contact their insurer themselves, according to the case manager. This generates another common problem since the 800-number on the back of an insurance card directs a patient to the insurer’s member relations department. Member relations will tell the patient the basics of their plan—namely, “Of course, you have the right to rehabilitation care.” Unfortunately, the utilization review department of the insurer is the one making the authorization denial – and the two departments rarely talk.
“So the patient loses trust in us, the people caring for them, because they do not believe what we are saying,” the case manager says. “It puts strain on the relationship between the hospital and the patient, it puts strain on the patient because they have to stay in the hospital, and it puts strain on us because we’re trying desperately to do right by patients.”
Solutions to the Problem
The case managers said much of the problem could be erased by two main actions. First, expanding an insurance company’s network of post-acute providers would allow a hospital to find a bed across the state that a patient’s insurer covers, thereby removing the fear of the patient paying out-of-network penalties or paying for their care entirely out-of-pocket.
But more importantly is the standardization of how to submit prior authorizations to the various insurers, and how quickly they are required to respond. Beginning in January 2026, under new federal guidelines, the timeframes for Medicare Advantage insurers to respond to prior authorization requests from providers will be reduced from 14 calendar days to 7 calendar days for standard requests while expedited requests remain at 72 hours. MHA recently wrote to the Centers for Medicare & Medicaid Services saying that even a 72-hour turnaround is too long – and the case managers agree.
But how about the argument that the insurers, although sometimes delayed in their responses, serve the important purpose of keeping costs in check?
“Prior authorization themselves are not the problem; it’s the processes associated with them,” said one case manager from the interviewed hospital. “The insurance company is not physically at the bedside assessing the patient, so they have to rely on our clinical professionals. The insurers require a physical therapy evaluation, an assessment, and we provide that to them when we make a transfer request. We are physically with the patient doing that assessment; the insurance company isn’t. We can see that the patient is not able to ambulate and cannot safely go home; the insurance company can’t.”
The case manager noted that if the patient didn’t have a Medicare Advantage insurer and had traditional Medicare instead, the transfer likely would be approved. “Medicare Advantage insurers are required by law to provide the same if not more services than traditional Medicare, but they often do not,” the case manager said. “And they’re doing a disservice to their patients by restricting them and causing long delays in getting to the next site of care.”
Enhancing Hospital-to-Home to Ease Capacity Crunch
While attempts to resolve the insurer prior authorization problem continues, the Healey Administration last week took another path to ease the capacity crisis: using American Rescue Plan Act Home and Community-Based Services funding to award $1.1 million to hospital and Aging Services Access Points (ASAPs) to expand the Hospital-to-Home Partnership Program.
The program helps discharge patients to their homes rather than to skilled nursing facilities or other post-acute settings. Determining the best location for a patient’s post-acute-hospital care is still left to the discretion of the patient’s care team.
There are currently 24 ASAPs across the state that help those over age 60 with care options, nutrition, food security, housing, financial wellness, transportation, and safety.
The following received grants of up to $300,000:
- Elder Services of Cape Cod and the Islands in partnership with Cape Cod Healthcare
- Mystic Valley Elder Services in partnership with Winchester Hospital
- Elder Services of Berkshire County in partnership with Berkshire Health Systems
- Highland Valley Elder Services in partnership with Cooley Dickinson Hospital
- AgeSpan, Inc. in partnership with Salem Hospital
Minuteman Senior Services in partnership with Emerson Hospital.
A Quick Fix That Works: Grad Nurse Regulations Issued
Another example of an action that is making a profound difference in addressing the state’s workforce and capacity crises is the law that the legislature passed and Governor Healey signed in April, allowing graduate nurses to practice at the bedside as they wait to take their NCLEX licensing exams.
That provision for the graduate nurses, and for nursing students in the final semester, was included in the FY2024 Supplemental Budget Act. It codified a regulatory flexibility that had been created during the pandemic to help hospitals deal with the influx of patients and workforce shortages. Post-pandemic, the flexibility continued to be invaluable as capacity pressures continue throughout the system.
Last week, the Board of Registration in Nursing and Bureau of Health Care Safety and Quality issued guidance to implement the law and to clarify the responsibilities of graduates, students, licensed healthcare facilities, and licensed healthcare providers. Among the provisions in the guidance is a requirement that the new nurses must take their licensing exam within one year after being hired by a provider; they must be supervised while working; and if they ultimately fail the NCLEX, they can no longer practice as a graduate nurse.
HHS Clarifies that Change is Responsible for HIPAA Breach Notifications
On May 31, the Department of Health and Human Services’ Office for Civil Rights (OCR) updated its FAQs webpage concerning the Change Healthcare cybersecurity incident. The update provided guidance on compliance with Health Insurance Portability and Accountability Act (HIPAA) rules and the necessary breach notifications following the Change Healthcare attack.
The updated FAQs clarify that hospitals and other entities affected by the attack can “delegate” the HIPAA-required breach notification to Change Healthcare or can complete the notification themselves. OCR emphasized the importance of notifying affected individuals, so they are informed about the breach’s effect on their protected health information. The OCR made the change regarding notifications after the American Hospital Association and other providers groups objected strongly to the original FAQ, which appeared to shift notification responsibilities from Change’s parent UnitedHealth Group, whose security shortcomings were responsible for the data theft, to the providers who have lost millions of dollars in revenue due to the breach.
Report Details How Mass. Can Lead in Healthcare AI
The Massachusetts High Technology’s Council’s “MassVision2050” initiative to advance the state’s global economic leadership last week released a report entitled Becoming the Global Leader in Applied AI for Healthcare & Life Sciences.
The report analyzes how AI (artificial intelligence) can revolutionize healthcare by accelerating innovation and improving patient outcomes.
In February Governor Healey signed an executive order creating the Artificial Intelligence Strategic Task Force to create specific recommendations for how the state can best support AI adoption in leading sectors. The High Tech Council’s report supplements that effort.
Peter Healy, the president of Beth Israel Deaconess Medical Center and a member of the MHA Board of Trustees was one of 13 members of the senior advisory council advising the Council on the report.
“The potential of AI in healthcare is immense,” Healy said. “This whitepaper showcases opportunities for advancing patient care, reducing administrative burden, and supporting clinical decision-making. The recommendations ensure Massachusetts amplifies its leadership in healthcare and technology, driving better patient outcomes and health equity. This project is pivotal for healthcare providers and hospitals in addressing today’s complex challenges.”

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association