Redeterminations Update; Senators Criticize Steward

INSIDE THE ISSUE
> MassHealth Redeterminations
> Senators Rap Steward
> Another Cyber Attack
> Mpox
> BMC Hospital at Home
> Drug Shortages
MONDAY REPORT
Massive MassHealth Enrollment Redetermination Effort Near Complete
For the past year, Medicaid agencies across the country have been verifying beneficiary eligibility for their entire Medicaid populations in accordance with state and federal requirements. This eligibility redetermination effort was required following a period of eligibility protections afforded to Medicaid enrollees during the COVID-19 public health emergency. Federal rules adopted last year required these redeterminations to begin in April 2023 and be completed by June 2024.
In Massachusetts, the Executive Office of Health and Human Services (EOHHS) initiated a comprehensive outreach campaign to educate MassHealth beneficiaries on the eligibility redetermination process and worked closely with patient groups, healthcare providers, and health plans to support the significant work involved with verifying eligibility for more than 2 million MassHealth members. Across the commonwealth, the state coordinated a communication plan, supported members in verifying eligibility, assisted individuals no longer eligible to obtain subsidized insurance through the Health Connector, and led numerous efforts to ensure coverage was preserved for eligible members. Health Care For All helped to lead a focused effort to mobilize direct outreach in communities with the highest number of MassHealth members. Hospital financial counselors played a significant role as well, serving as state “Certified Application Counselors” to help patients navigate the complex application and eligibility process.
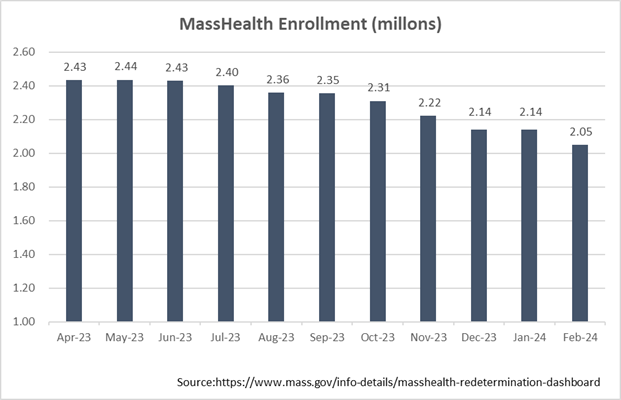
With all redeterminations initiated, MassHealth enrollment has decreased substantially, and stood at 2.05 million members at the end of February. Compared to April 1, 2023, enrollment is down by approximately 350,000 members – a 14.7% decrease. Current MassHealth enrollment remains higher than pre-pandemic levels when the program covered 1.76 million people in February 2020. Through February of this year, the state’s Health Connector has enrolled about 108,000 individuals who were deemed no longer eligible for MassHealth. According to EOHHS, this represents approximately one quarter of those determined no longer eligible for MassHealth through the redetermination process.
MassHealth expects to see additional departures in the months ahead as new data emerges and as more members complete the full renewal process. Eligibility redeterminations will also continue as usual going forward. With the reductions, hospitals are watchful of the effects on low-income populations and whether there will be an effect on the state’s uninsured fund – the Health Safety Net. That program is currently experiencing a funding deficiency that MHA estimates to be more than $140 million, which is entirely financed by acute care hospitals.
U.S. Senate Hearing Targets Steward and Private Equity’s Healthcare Role
Massachusetts’ U.S. Senators Edward Markey and Elizabeth Warren during a hearing last Wednesday at the State House slammed Steward Health Care, its CEO Ralph de la Torre, and, more broadly, the use of private equity investments in the healthcare system.
The field hearing of the Senate’s Health, Education, Labor and Pensions Committee’s Subcommittee on Primary Health and Retirement Security, which Markey chairs, was entitled “When Health Care Becomes Wealth Care: How Corporate Greed Puts Patient Care and Health Workers at Risk.”
No one from Steward attended although an invitation was extended to de la Torre, who Warren called “cowardly” for not attending, while accusing him of “looting” Steward’s Massachusetts hospitals.
“Turning private equity loose in our healthcare system kills people,” Warren said. And while most of the hearing focused on the well-known details of how profits were extracted from the Steward health system, whose hospitals were then saddled with excessive rents, some of the hearing focused on the recently announced proposal by Optum to buy Steward’s physician practice.
Warren called the M.D. group the final Steward asset of value. “But the [Optum] deal provides no guarantee that the hospitals would stay open – none,” she said. “In fact, the money could go into Steward and right back out the door again to corporate lenders and investors without a single penny used to help these hospitals.” She added that Optum “has run this same play in other states. Optum boosts its profits by overbilling Medicare and cutting care for the patients who need it most. I don’t understand how regulators can approve such a deal.”
“MHA members support a close examination of private equity’s role in our system,” said MHA President and CEO Steve Walsh in the wake of recent government hearings. “Now is the time to create clear guardrails for these entities to ensure financial motives never put the mission of affordable, equitable, and worker-empowered care at risk. As we imagine the future of healthcare, there is a role for private dollars seeking to innovate and improve patient care delivery. But these transactions should be managed in partnership with trusted local providers and be held to the same oversight and transparency standards that every hospital has committed to. We thank our local and federal policymakers for placing well-deserved attention on this issue.”
As part of the hearing, Markey announced a discussion draft of his Health Over Wealth Act that would, among other things, require private equity to set aside funds to protect access to care and direct the Department of Health and Human Services to block real estate deals that threaten to destabilize healthcare systems.
Warren also discussed the need for private equity legislation. In the past, she has introduced her Stop Wall Street Looting Act. She said that bill contains elements along with other proposed federal legislation that, if not passed nationally, could be adopted by state legislatures to limit the role of private equity in healthcare.
New Warning About Financial Cyber Scheme
As effects from the Change Healthcare cyberattack still reverberate throughout the healthcare system, the American Hospital Association and cyber experts are warning providers of a new specified threat that is targeting health system employees that have sensitive financial roles.
“The scheme involves what is presumably a foreign-based threat actor calling IT help desks and leveraging stolen personally identifiable information of employees to answer security questions posed by the IT help desk,” AHA writes. “The threat actor then requests a password reset and requests to enroll a new device, such as a cell phone, to receive multi-factor authentication codes. This new device will often have a local area code. This effectively defeats multi-factor authentication, including SMS text and higher level ‘phishing-resistant’ multi-factor authentication, to provide full access to the compromised employee’s email account and other applications.” The cyberattackers then use the employee’s compromised e-mail account to change payment instructions and divert funds out of a system or to insert malware.
Help desks around the U.S. are cracking down on password resets, AHA reports, including making employees requesting help to appear in person at the help desk as opposed to calling in for tech support.
DPH to Providers: Remain Vigilant About Mpox
In a clinical advisory issued last week from the Department of Public Health, the state notes that mpox incidence in Massachusetts has increased from October 2023 to March 2024, and that providers should be vigilant for the viral disease in people with potential exposure, including previously vaccinated individuals.
DPH expressed concern about a “concurrent but geographically distinct” outbreak of mpox now occurring in central Africa and urged that specimens collected from patients with travel history to central Africa or recent close contact with someone who recently travelled to central Africa should be sent to the state lab, rather than to a commercial laboratory for testing.
There have been 32 confirmed or probable cases in Massachusetts reported from October 2023 to date.
BMC Hospital at Home
Boston Medical Center (BMC) has launched a Hospital at Home service that provides eligible patients with inpatient-level healthcare in the home. BMC is the twentieth hospital in Massachusetts to receive authorization from the Centers for Medicare and Medicaid Services to conduct a hospital at home program.
BMC says the service is a physician-led, remote acute care unit that monitors patients around the clock, provides daily M.D. e-visits, and easy access to a dedicated care team.
“Once enrolled in the remote acute care unit, patients are equipped with an advanced virtual hospital room kit, including app- and web-based technology to facilitate all medical monitoring, scheduling of in-home visits, and connectivity with providers in real time, providing all the same services patients would receive during a traditional hospital stay and held to the same rigorous standards for quality,” according to a BMC media release.
Such hospital at home programs are gaining wider acceptance in the United States as studies have shown outcomes and patient satisfaction improve and healthcare costs decrease with their use. They have also been celebrated for their role in keeping patients out of emergency departments and easing the capacity pressures that hospitals are under. MHA and its members have long advocated for insurance coverage of these services.
“Providing hospital-level care in a patient’s home allows us to increase patient access to care options, expand hospital capacity and provide high-quality care to more of our community without additional strain on our resources,” BMC Health System President & CEO Alastair Bell, M.D. said.
HHS Releases Drug Shortage Strategy Advancing Role of Hospitals
Last Tuesday, U.S. Health and Human Services (HHS) released a white paper entitled Policy Considerations to Prevent Drug Shortages and Mitigate Supply Chain Vulnerabilities in the United States.
The report reviews steps HHS has taken to prevent drug shortages, such as establishing a new Supply Chain Resilience and Shortage Coordinator role and bolstering the Food and Drug Administration’s capacity to minimize or prevent shortages through increased access to data.
Among the additional proposals that policymakers should consider, HHS proposes working with Congress to create and implement a Manufacturer Resiliency Assessment Program (MRAP) and a Hospital Resilient Supply Program (HRSP). The MARP “could measure resilience of manufacturers and bring transparency to the prescription drug supplier base” and the HRSP could bolster demand by “[establishing] demand incentives and/or penalties, facilitating hospital purchasing that prioritizes supply chain resilience, rather than the current structure which generally prioritizes cost alone.” The HSRP would use Medicare payments and penalties to incentivize hospitals to prioritize quality management and supply chain reliability when purchasing drugs – a proposal garnering a great deal of attention from the hospital community.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association