MHA Report: Health System Challenges & Solutions

INSIDE THE ISSUE
> MHA Report
> The House’s Health Reform Bill
> State Senate FY2025 Budget
> National Hospital Report
> Patient & Family Advisory Councils
> MOLST to POLST
> tMED’s Telehealth Letter to Congress
> UHG Criticized
> Transition
MONDAY REPORT
MHA Report Outlines Health System Challenges, Offers Solutions
As many patients in Massachusetts continue to experience long wait times and obstacles to their care, MHA has issued a new report outlining the relentless challenges the healthcare system faces and offering some achievable goals to relieve the pressures on patients, caregivers, and employers.
MHA’s Causes & Consequences: Inside the Healthcare Crisis analyzes the growing stresses within the healthcare system, which the report notes “is fundamentally different than it was before COVID-19 began.” It explains how the problems escalated so quickly, introduces new data showing $400 million in annual losses related to unreimbursed care, and offers solutions on what can be done to set Massachusetts on a path to recovery.

The report ties together the health system’s well-documented existing problems, from tens of thousands of workforce vacancies, to patient backups that result in “stuck patients” and emergency department boarding, to incidents of abuse and violence against caregivers that lead to burnout, to overall financial stability in which 75% of hospital health systems are operating on negative margins. It also sheds light on the changing nature of the patient population, which is generally sicker, older, and in need of longer hospital stays than before the pandemic.
New data in the report shows how the stuck patient crisis – that is, 1,000 or more patients unable to transition to the next level of care on any given day – is costing hospitals $400 million annually. Because commercial insurers pay hospitals a fixed per-patient, per-diagnosis amount, hospitals receive little to no additional payment for accommodating patients that cannot transition to the next level of care. The $400 million annual loss does not include the lost revenue that accumulates when hospitals cannot accept new patients due to beds filled with stuck patients.
“For Massachusetts hospitals and caregivers, the crisis brought on by COVID-19 never ended – in fact, it has only intensified. They are in need of support more than ever.” said Steve Walsh, president & CEO of MHA. “Fortunately, there are solutions within our grasp. We hope this is a helpful resource for legislators and our partners across healthcare as they pursue policies and innovations that can help provider organizations recover.”
Hospitals across the U.S. are facing a similar set of circumstances affecting their operations. Last week, the American Hospital Association (AHA) released a report (see below) showing how stagnant reimbursements are harming hospitals that are experiencing substantial challenges due to higher costs for the labor, drugs, and supplies that go into patient care. What sets Massachusetts apart, Walsh said based on his discussions with his peers across the country, is that the Massachusetts health ecosystem of providers, insurers, state government, patient advocates, and others has proven consistently that it can “collaborate and reinvent what accessible care looks like for patients across the commonwealth.”
For example, to help resolve the workforce crisis, the legislature could pass legislation (H.1211/S.747) to allow Massachusetts to join the Nurse Licensure Compact, as well as passing comprehensive workplace violence legislation (H.2381/S.1538).
Among the other solutions detailed in Causes & Consequences is funding a Complex Care Ombudsman Program to assist with patient transitions, and strengthening telehealth to allow the expansion of care outside of hospitals. Hospitals also support sensible reforms to insurers’ prior authorization processes, which often cause care delays, accelerate caregiver burnout, and result in hundreds of millions of dollars in cost waste across the healthcare system. MHA, the Massachusetts Medical Society, and Health Care For All have come together to champion legislation that streamlines or eliminates low-value prior authorization requirements (H.1143/S.1249).
The House’s Ambitious Healthcare Reform Bill
The Massachusetts House is moving forward on a comprehensive healthcare reform bill that, among other things, seeks to rebuild the healthcare cost growth benchmark process, segments out health insurance companies from Division of Insurance oversight by creating a new Division of Health Insurance, and empowers the Health Policy Commission (HPC) to create a rate equity target to improve insurer reimbursements to hospitals serving “priority populations.”
The bill – H.4620, An Act Enhancing the Market Review Process – emerged last Tuesday from the Health Care Financing Committee chaired by John Lawn (D-Watertown) and was immediately endorsed by House Speaker Ron Mariano, signaling its prospects for a House vote before the session ends in July are good.
Among the bill’s many moving parts is one for which MHA has long advocated – revamping the process by which the HPC sets the annual healthcare cost growth benchmark. H.4620 maintains that the state’s benchmark will be based on the growth rate of the potential gross state product – the long-run average growth rate of the commonwealth’s economy excluding fluctuations due to the business cycle. For the last decade, this has been projected each year to be 3.6%. New in the House bill is a potential adjustment factor to this growth rate that must be approved by both a new technical advisory committee and the HPC board. Measurement of cost growth relative to the benchmark would now be based on 3-year cycle. MHA has argued the benchmark should reflect near term spikes in spending due to inflation, or specific events like pandemics, workforce shortages, or hospital system closures.
The bill also expands the types of healthcare organizations that would fall under the purview of the HPC and the Center for Health Information and Analysis (CHIA) and it assesses these “non-hospital providers,” including clinical labs, imaging facilities, and urgent care centers, to help pay for the HPC’s and CHIA’s budgets. The number of HPC commissioners would be reduced from 11 to nine.
Spurred by the Steward Health Care debacle, the bill creates new oversight and requirements for private equity investors, healthcare real estate investment trusts, and management services organizations. It gives the HPC authority to investigate real estate sale lease-back arrangements, and the conversion of a provider or payer from a non-profit to a for-profit entity. The out-of-state parents of a Massachusetts provider organization, or the organization’s significant equity investors, would have to disclose their audited financial statements under provisions in the bill.
The Senate’s health-related bill this session – S.2499, An Act Relative to Pharmaceutical Access, Costs and Transparency, or PACT Act 3.0 – passed the upper chamber unanimously in November 2023. How and if the House and Senate will resolve that bill, as well as H.4620, before the session ends remains to be seen.
Senate State Budget Proposal Expected Tomorrow
The Massachusetts State Senate is expected to release its FY2025 state budget proposal tomorrow. The House passed its $58 billion budget proposal on April 26. That budget contained important technical amendments that allowed a joint MHA-Executive Office of Health & Human Services hospital assessment plan to move forward. Under the plan, which the Senate must still approve, the annual assessment on hospitals increases but the net benefit in federal funds flowing back to Massachusetts and to hospitals – especially safety net hospitals — also increases.
AHA Report Outlines State of Hospitals Nationally
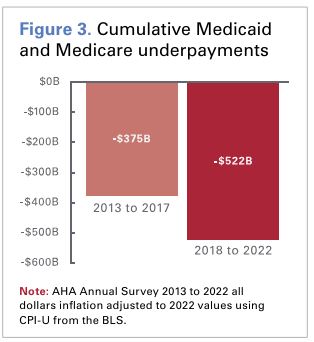
A new report from the American Hospital Association shows that hospitals nationally face rising costs for workers, pharmaceuticals, and supplies while government reimbursements remain stagnant and commercial insurance company policies stack administrative burdens upon them.
“Taken together, these issues have created an environment of financial uncertainty where many hospitals and health systems are operating with little to no margin,” AHA writes. “While recent data suggest that some hospital and health system finances have experienced modest stabilization from historic lows in 2022, the hospital field is still far from where it needs to be to meet the demand for care, invest in new and promising technologies and interventions, and stand ready for the next healthcare crisis.”
The well-sourced report calls on Congress to, among other suggestions, resist any further Medicare and Medicaid cuts, protect the 340B drug pricing program, and take actions to hold commercial insurers accountable for practices that delay, deny, and disrupt care.
Patient and Family Advisory Councils Spring Forum 2024
The Betsy Lehman Center for Patient Safety is expanding efforts to support the work of patient and family advisory councils (PFACs) in Massachusetts healthcare settings. Last fall, the center assumed the responsibility previously held by Health Care For All for collecting and sharing PFAC annual reports. As a next step, to promote engagement among councils, the center will host an inaugural virtual forum on Thursday, May 30 from 5 to 6:30 p.m. Members of all hospital PFACs in Massachusetts are invited to attend the event entitled Creating Connections for PFAC Impact: Diversifying Membership and Engaging with Leadership. More information about the Betsy Lehman Center’s PFAC activities, plus a registration form for the May 30 forum is here.
MOLST-to-POLST Info Session Tomorrow
The state effort is still underway to change the way patients facing serious medical events inform their caregivers about their care decisions. The state is switching from the Medical Order for Life-Sustaining Treatment (MOLST) form to the POLST form, which stands for Portable Orders for Life Sustaining Treatment. One of the main differences is that the POLST form can be submitted and accessed electronically. Tomorrow the state is holding an information session for senior healthcare executives on the MOLST-to-POLST transition. MHA last week informed its membership about the forum. E-mail Priscilla Ross, R.N., POLST program director, at priscilla.ross2@mass.gov, for more information.
Coalition Outlines Clear Path to Telehealth Success
Telehealth is a proven tool for expanding access to healthcare services, especially in rural and underserved areas, and for patients with mobility issues or with other limitations that prevent them from accessing in-person care in a timely manner. But roadblocks still exist preventing telehealth from reaching its full potential to assist patients and caregivers.
Last week, the tMed Coalition, representing more than 50 organizations and led by MHA, wrote to the Massachusetts Congressional delegation, outlining priority areas that would strengthen telehealth.
Among the suggestions, tMed urged extending the Hospital at Home waiver beyond its December 31, 2024, expiration date; allowing more practitioners such as occupational and physical therapists, speech-language pathologists, and audiologists to furnish telehealth services; extending coverage and payment for audio-only telehealth services; and changing the rules to make it easier for mental health patients to access telehealth services.
“Without clear guidance from Congress on a long-term approach for telehealth flexibilities, healthcare delivery systems will not be able to invest sufficient resources to allow maximal access to patients,” the coalition wrote. “We believe that policymakers now have more than enough evidence to see the benefits of telehealth and consider a permanent pathway to ensure that telehealth continues to be available and accessible.”
UnitedHealth Group Criticized at Congressional Hearing
The CEO of UnitedHealth Group (UHG) Andrew Witty appeared before the Senate Finance Committee last week and was severely criticized by Senators on both sides of the aisle, not only for UHG’s failure to prevent a data breach that is still disrupting the nation’s healthcare system, but for the fact that UHG is just too large.
UHG is parent of the nation’s largest health insurer, UnitedHealth Care, as well as parent of Change Healthcare that was hacked in February. UHG owns Optum, which controls about 10% of all physicians in the U.S. and is currently negotiating with Steward Health Care to purchase Steward’s physician practices. UHG also owns the large pharmacy benefit manager OptumRx, among other parts of its portfolio which generated $372 billion in revenue in 2023.
“The Change hack is a dire warning about the consequences of ‘too big to fail’ mega-corporations gobbling up larger and larger shares of the healthcare system,” Senator Ron Wyden (D-Ore.) said.
Massachusetts Senator Elizabeth Warren (D) said UHG’s control of many aspects of the healthcare system was dangerous.
“Because UnitedHealth has brought up every link in the healthcare chain, you are now in a position to jack up prices, squeeze competitors, hide revenues, and pressure doctors to put profits ahead of patients,” Warren said to Witty. “UnitedHealth is a monopoly on steroids.” Noting that the UHG data breach resulted in losses to providers, Warren said, “UnitedHealth is using its own data breach to snap up doctors’ practices that have been driven to the edge of bankruptcy by that same data breach … UnitedHealth will stop at nothing to grow bigger, bigger, and bigger as we speak. UnitedHealth is trying to pick the bones of Steward Health Care in my home state of Massachusetts.”
UHG’s Witty also addressed a major concern among providers regarding the fact that while Change’s processing systems were down during the breach, care decisions proceeded without the proper prior authorizations from insurers. Providers want to ensure that insurers do not now attempt to refuse coverage for such care. Witty assured Sen. Bill Cassidy (R-La.) that UHG’s insurance arm would not attempt any claw backs on those care decisions. If another, non-UHG insurer that used Change systems attempted to refuse coverage because a prior authorization was not completed during the breach, Witty said, “We will cover that.”
While an attack by a foreign adversary that disrupts the nation’s healthcare system normally would be met with sympathy, UHG’s failure to have even the most basic multi-factor authentication on its systems drew ridicule. (Multi-factor authentication requires a person logging in to provide more than their password; an example would be a utility company texting a homeowner a five-digit code that has to be entered before the person pays a bill.)
Senator Thom Tillis (R-N.C.) said of UHG’s security errors, “This is some basic stuff that was missed.” Tillis held up a book entitled “Hacking for Dummies” to illustrate his point.
Transition
Steve Landers, M.D., who has served as president & CEO of Hebrew SeniorLife since July 2023, announced last week that he is stepping down from the post, effective May 17. HSL noted in a media release that “it became evident that relocation to Boston from New Jersey was not the best option for his family at this time.” Lou Woolf, who led Hebrew SeniorLife for 14 years before Landers, is coming back as interim president & CEO until a permanent leader is found. Woolf is a former member of the MHA Board of Trustees and served as the inaugural Chair of its Continuum of Care Council.


 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association