Maternal Health, Climate Change, and more …

INSIDE THE ISSUE
> Maternal Health Bill
> Health & Climate
> AMA Raps Prior Authorizations
> Residual Effects of Change Cyberattack
MONDAY REPORT
House Passes Comprehensive Maternal Care Bill
The Massachusetts House unanimously passed a sweeping maternal health bill last Thursday that will, among other things, create a Board of Midwifery under the Department of Public Health (DPH) to oversee licensure; require midwives to carry a Certified Professional Midwife credential; permit licensed midwives to administer lifesaving medications; and include licensed midwives as MassHealth providers.
H.4773, An Act promoting access to midwifery care and out-of-hospital birth options also allows midwives to attend to a patient who has received abortion-related care. Additionally, the bill requires DPH to promulgate regulations for freestanding birth centers, including how they will transfer a patient to a nearby hospital as needed for emergency treatment beyond that provided by the birth center. Freestanding birth centers would have an administrative director responsible for implementing and overseeing the operational policies of the birth center, and a director of clinical affairs on staff who is either a certified nurse-midwife or physician.
The bill also requires DPH to establish a program to conduct an in-depth fetal and infant mortality review to identify social, economic, and systemic factors associated with the deaths.
“At a time when access to reproductive healthcare is under assault, where some states, along with the Supreme Court, are creating barriers or eliminating access to reproductive healthcare, Massachusetts continues to strengthen our resolve to protect and expand access to reproductive care,” said Rep. Marjorie Decker (D-Cambridge) upon passage of the bill, as reported by State House News Service. Decker, who co-chairs the legislature’s Public Health Committee, was integral to the design and passage of the bill.
H.4773 also establishes a task force on maternal health access and birthing patient safety to study the current status of services across regions of the commonwealth and among birthing patient populations. MHA would have a seat on that task force, which is also tasked with studying the essential service closure process, the maternal healthcare workforce, and methods to increase investments in maternal healthcare. Additionally, the task force will look at past essential service closures for inpatient maternity units and acute-level birthing centers, and closures of community-based, office-based and preventative maternal healthcare.
The bill requires postpartum depression screening coverage by MassHealth and private payers. It also creates licensure pathways for lactation consultants and expands access to lactation support services.
“Across the nation, maternal health has emerged as a pressing access issue, workforce issue, and basic patient rights issue,” said Mike Sroczynski, executive vice president and general counsel at MHA. “Our local leaders are once again stepping up to meet the moment. These reforms can make a meaningful difference to everyone who is in need of – or has committed their life to delivering – safe and equitable maternal care. We applaud Chair Decker and House leadership for making this a priority on behalf of patients and caregivers in Massachusetts.”
MHA Weighs in With Budget Conference Committee
The Conference Committee tasked with resolving difference between the House and Senate state budget proposals, and getting a final document to Governor Maura Healey before the July 31 close of the fiscal year, is currently meeting at the State House.
Last week, MHA sent a letter to the conferees laying out budget priorities for the hospital and healthcare communities.
The biggest priority for MHA’s membership is for the two bodies to agree on a newly designed hospital assessment that aligns with the recent MHA and Executive Office of Health and Human Services proposal. That plan increases the tax on hospitals but ultimately results in more federal dollars flowing back to the state in federal Medicaid funding. While both chambers approved the overall plan, the Senate proposal left out language relating to Cambridge Health Alliance’s (CHA’s) special designation as a “public hospital.” MHA respectfully asked that the Senate approve the House language, which would help CHA at no cost to the General Fund.
MHA asked conferees to keep in mind a series of urgent financial considerations as they addressed the budget, each of which could further destabilize the provider community in Massachusetts. Specifically of concern, Governor Healey’s FY2025 MassHealth budget assumed $300 million in payment reductions, an assumption that has been carried forward in the House and Senate budgets. The Executive Office of Health and Human Services (EOHHS) indicated that the hospital portion of those cuts could reach $100 million and the agency plans to soon share its proposal to implement the cuts in the upcoming RY2025 acute hospital RFA. MassHealth Accountable Care Organization and Managed Care Organization rates are also expected to absorb the payment reductions.
MHA also raised alarm with funding deficiencies in the Health Safety Net program that are expected to exceed levels not experienced since prior to the state’s historic 2006 healthcare reform law; the safety net shortfall is anticipated to exceed $210 million in FY2024. The system, as currently designed, would leave hospitals on their own to covering these historic shortfalls.
Among other MHA requests is one asking conferees to adopt a proposal in the Senate budget that would require the Division of Insurance to issue a report on how health insurance companies are implementing mental health parity mandates. Parity ensures that individuals with mental health conditions receive equitable access to diagnosis, treatment, and support services. In the report, DOI is tasked to review consumer complaints alleging health insurer non-compliance.
State, and MHA, Focus on Climate
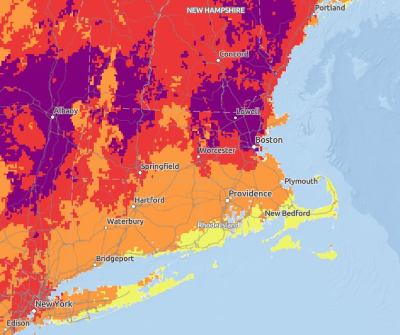
Coinciding with last week’s heat wave across much of New England, the state has announced its new toolkit that not only provides extreme heat forecast information but helps alert healthcare interests to prepare for a response.
The Heat Education and Alert Tools (HEAT) response is a collaboration between the state’s Bureau of Climate and Environmental Health, Office of Preparedness and Emergency Management, and Office of Local and Regional Health. Its main component is the National Weather Service’s Heat Risk Tool that forecasts various levels of heat through a color-coded map that assesses, among other things, how the climate will affect healthcare systems.
The Massachusetts page contains community profiles for each city and town in the commonwealth, which shows how environmental issues, including climate, can affect certain populations.
In announcing the new effort, DPH’s Bureau of Climate and Environmental Health wrote, “This effort will help to protect our communities from the adverse effects of extreme heat and better prepare our healthcare sector, local health departments, and communities to respond to extreme heat events and the climate crisis. By partnering with a broad range of stakeholders and leveraging our evidence-based resources, Massachusetts can position itself as a leader addressing the serious threat to public health caused by climate change. If we face this climate crisis together, we can build capacity, instill resiliency, especially for our most vulnerable communities, and protect the public’s health.”
This month, MHA announced the creation of a new Hospital Climate Sustainability Workgroup that will play a key role in informing the association’s advocacy on potential state and federal policies related to climate sustainability. Already, many state and federal regulatory authorities which oversee healthcare, in addition to provider organizations themselves, are incorporating climate priorities into their work. And non-government entities, such as The Joint Commission (TJC), are also focusing on the intersection of health and climate. In January, TJC announced a voluntary Sustainable Healthcare Certification program for hospitals seeking to accelerate their sustainable practices and reduce greenhouse gas emissions.
National Physicians’ Group: Excessive Prior Auths Harm Patients, M.D.s
Local and national hospitals have long complained about onerous health insurance company prior authorization (PA) processes that in Massachusetts have been tied to the lengthy delays in transferring patients from the acute care setting to post-acute care, among other caregiving and worker wellbeing problems.
Now the national physicians’ group – the American Medical Association (AMA) – has weighed in with its own complaints about prior auth.
Last week the AMA released results of its survey of 1,000 physicians (400 primary care/600 specialists) from different practice settings, which found that the prior auth process “continues to have a devastating effect on patient outcomes, physician burnout, and employee productivity.”
Ninety-four percent of doctors say waiting for an insurer to make a prior auth decision delays care, and 78% found that the delays have resulted in a patient abandoning treatment.
Ninety-three percent of doctors say PA decisions have a negative effect on patient care; 35% say the decisions are “rarely or never evidence-based;” and 24% of the survey respondents report that prior auth has led to a serious adverse event for patients in their care.
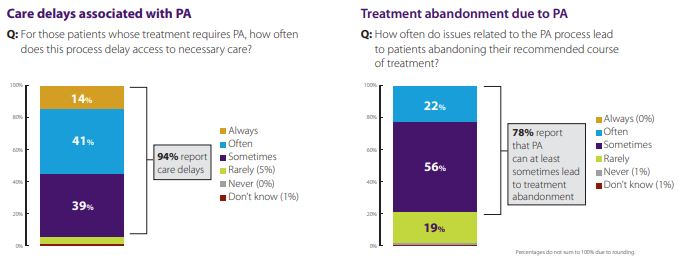
As for the effect on physicians themselves, the survey showed that the average M.D. practice must deal with 43 PAs per physician, that a third of them must hire a specific worker to handle the influx of PA requests, and that 95% feel the PA process somewhat or significantly increases physician burnout.
When there is a dispute over a prior auth decision, a “peer-to-peer review” often follows, but only 15% of doctors participating in these burdensome phone calls feel that the insurer’s “peer” often or always has the appropriate qualifications to make a medical decision.
MHA has filed legislation jointly with the Massachusetts Medical Society and Health Care For All that would address some of the difficulties patients and providers encounter from commercial health insurance companies’ prior authorization policies. The legislation would not eliminate prior auth, but under the MHA-MMS-HCFA proposal, the processes would be streamlined. Among other things, there would be greater transparency around denials and appeals, continuity of care provisions for courses of treatment without having to constantly seek new prior authorizations, and adoption of electronic prior authorization to go along with CMS requirements that will be going into effect in 2026 for Medicare Advantage plans.
Despite its broad support from Massachusetts healthcare providers and patient advocates, the legislation still faces heavy opposition from the local insurance industry, which argued last week that “emerging technologies” can – eventually – serve as the fix for prior auth delays.
Change Healthcare Issue Subsides, But Still Exists
The Centers for Medicare and Medicaid Services (CMS) said last week that effective July 12 it will no longer issue Accelerated and Advance Payments to providers that were affected by the Change Healthcare data breach. But the federal government, noting some residual effects from the Change cyberattack, is giving providers more time to dispute billing under the No Surprises Act.
CMS’s advanced Medicare payments have eased cash flow disruptions to providers affected by the cyberattack that took the Change electronic data interchange offline in February. CMS said it has made nearly 9,000 advance payments, totaling more than $3.2 billion – and has recovered more than 96% of those payments now that systems are up and running again.
If billing problems persist after the July 12 cutoff date, CMS says, then providers should contact Change Healthcare, owned by UnitedHealth Group, and/or their Medicare Administrative Contractor (MAC).
In a related note, the Departments of Health and Human Services, Labor, and the Treasury issued a statement last week saying that the Change cyberattack has disrupted the No Surprises Act negotiation process. The No Surprises Act, among other things, sets up a dispute resolution process for providers and insurers that disagree over payments for out-of-network emergency services medical bills. Part one of that process is initiating open negotiation. But the federal departments conceded last week that many providers can’t begin the negotiation step because they have not received necessary payment information from insurers due to the Change Healthcare cybersecurity incident.
As a result, any provider that has not been able to open a negotiation with an insurer due to the Change event now has until October 12, 2024, to do so. Providers must first attest to the fact that their inability to initiate open negotiation is directly attributable to the cyberattack.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association