Lousy Finances, Prior Auths Rapped, and more …

INSIDE THE ISSUE
> CHIA Report
> HPC Review of Steward
> Post-Acute Prior Auths
> TJC Recognition for Mass. Hospitals
> HELP Committee Vote
MONDAY REPORT
Hospitals Are in the Red; Administrative Burden is One Reason
The Center for Health Information & Analysis (CHIA) last week released its latest report detailing how the state’s health system finances changed between 2022 and 2023.
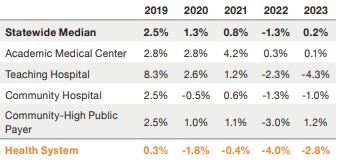
What might get lost in CHIA’s headline announcement that “hospital profitability increased 6.4 percentage points from 2022” is the fact that 2022 was the worst hospital financial performance year in recent history. Operating margins across the state were barely positive in fiscal year 2023 and that trend has worsened in 2024 with the statewide median operating margin now negative.
CHIA’s report released last Thursday covers hospital fiscal year 2023, which ran from October 1, 2022, to September 30, 2023. The report speaks to both total margins and operating margins. Total margins do not reflect the day-to-day operations of hospitals and health systems and include unrealized gains, or investment holdings. Operating margins track the difference between what hospitals spend to deliver care and the revenues they receive to support their operations.
The CHIA report on the state of the system beginning two years ago shows that the statewide acute hospital median operating margin was just 0.2% in 2023, with 48% of hospitals in the negative. But the most recent numbers – from March 2024 – show that the statewide acute hospital median operating margin is now negative, or -0.1%, with 50% operating in the red. Credit agencies require stronger operating margins for a facility to receive favorable interest rates for borrowing. Massachusetts margins have been hovering below or slightly above zero for years.
“While CHIA’s report paints a dismal picture for Massachusetts hospitals in 2023, financial conditions have only deteriorated further since then,” said MHA’s Senior Vice President of Healthcare Finance & Policy Dan McHale. “As of this March, hospitals’ median operating margin had once again dipped into the red, capping four years of unrelenting losses that have affected every aspect of care delivery. It is important that policymakers take notice when we have a system in which 50% of hospitals report negative operating margins, and 73% of hospital health systems – which include affiliated physician practices – are also in the red. That’s unsustainable.”
HPC Reviewing Stewardship and Hospital Proposals
In addition to the bankruptcy court in Texas’s approval of the new owners for Steward Health Care’s hospitals in Massachusetts, state and federal regulators must also sign off on the deals.
In Massachusetts that means filing a Material Change Notice with the Health Policy Commission (HPC) and Emergency Determination of Need applications with DPH. The three new buyers – Boston Medical Center, Lawrence General Hospital, and Lifespan – have indeed filed that paperwork.
At last Thursday’s HPC Board meeting, HPC staff told the commissioners that the reviews are underway and that they are cognizant of the hoped-for September 30 deadline to finalize the hospitals transfers.
While it reviews the hospital applications, the HPC is concurrently reviewing the purchase of Steward’s 2,900-plus physician practice, Stewardship, by the for-profit Rural Healthcare Group, a subsidiary of Kinderhook Industries.
Primary care physicians and specialists within a group practice are the entities that refer patients to hospitals. The physicians in turn practice within the hospitals. The choregraphed interaction between the two groups is essential to keep the health system operating. The purchase of Stewardship has raised more questions than answers.
What’s Rural Healthcare/Kinderhook’s long-term strategy in the state? Will Steward physicians who referred to Steward hospitals refer to the new owners? Will the new owners subsume the Steward physicians into their own practices? What will happen to the non-clinical personnel within the practices?
“I want to know, what are the ways that we can hold [Rural Healthcare] accountable for doing right by patients, doing right by the people of the commonwealth; what are the ways we’ll be able to do that over time?,” asked Alecia McGregor, PhD, assistant professor of health policy and politics at the Harvard T.H. Chan School of Public Health.
The HPC’s Director of Market Oversight and Monitoring Megan Wulff told commissioners last Thursday that the HPC is asking these questions and others in their talks with the for-profits. She said if the deal goes through, then the HPC would be able to bring the new owners under its cost trend review process. HPC Board Chair Deb Deveaux said that to date Rural/Kinderhook has been open in its discussions with the state and “know our concerns about private equity.”
AHA’s Letter on Prior Authorization Mirror Mass. Experiences
Regulations are now in effect to limit the arbitrary claims denials from Medicare Advantage plans, but across the U.S., health insurance companies continue to ignore the federal directives. That’s the gist of a 10-page letter that the American Hospital Association (AHA) sent last week to the U.S. Department of Health & Human Services’ Office of Inspector General.
The letter focused specifically on how some Medicare Advantage (MA) plans abuse their prior authorization authority when making determinations for post-acute care. Denying claims outright without offering reasons why; failing to list the names of the insurer’s physician making decisions, thereby making it difficult to challenge the review; and deliberately refusing patient transfers to post-acute facilities to keep cost down were among the MA practices the AHA cited.
“These abusive practices further strain healthcare delivery system resources and capacity at referring general acute-care hospitals by imposing days- or weeks-long delays in the necessary authorizations to transition patients to the next site of care, while sometimes precluding patient access to post-acute care sites altogether,” the AHA wrote.
Noting that some insurers are better than others, the AHA requested that the Inspector General focus her recently announced review on plans that “have a history of suspected or actual violations.”
Providers have consistently sounded the alarm about MA plans that deny authorization and then keep the reasons for the denial hidden, citing proprietary guidelines, which the AHA says is prohibited.
“CMS rules require transparency in internal coverage criteria and adherence to Medicare guidelines,” the AHA wrote. “This transparency cannot meaningfully be achieved if plans can just state the care is not medically necessary and cite the Medicare manual without analysis or justification.” And without a stated reason for the denial it becomes harder for providers and patients to appeal the decision.
The AHA also claimed that by refusing to transfer a patient to needed post-acute care, thereby forcing the patient to stay in an acute care hospital, the Medicare Advantage plans avoid paying for post-acute care, and do not have to pay the acute care hospitals additional reimbursement. That’s because the insurer “will have already paid the referring hospital a flat rate for care and would prefer to use the hospital to delay or avoid the patient’s discharge to the next site of care, which would require a separate, additional reimbursement.”
Insurer failures to authorize transfers of patients in Massachusetts is one of the leading reasons providers cite for the backup of thousands of patients in Massachusetts acute care hospitals and the resultant capacity crisis.
In June, MHA interviewed case managers from a Massachusetts health system to learn first-hand the day-to-day roadblocks providers face when attempting to transfer patients to post-acute care. The local challenges mirror the concerns the AHA voiced in its letter.
Southcoast and Lawrence General Lead the Way on Equity Certification
Southcoast Health and Lawrence General Hospital are the first two MHA member hospitals to successfully achieve The Joint Commission’s Health Care Equity Certification.
Massachusetts hospitals are in the midst of a nation-leading commitment to make healthcare more equitable. Through a historic five-year 1115 Medicaid Waiver, they have come together with the state to embed health equity efforts at the point of care, make services more accessible for patients, and reduce persistent disparities.
Last year, every Massachusetts hospital successfully achieved The Joint Commission’s Health Care Equity Accreditation – a first-in-the-nation accomplishment. Starting earlier this year, the hospitals are advancing to the next phase by achieving The Joint Commission’s more comprehensive Health Care Equity Certification. The certification consists of a rigorous review rooted in health equity principles across five domains: leadership, collaboration, data collection, provision of care, and performance improvement.
While Southcoast and Lawrence General are the first to achieve the designation, all Massachusetts hospital will eventually reach this status as part of the waiver process.
U.S. Senate Takes Next Step to Hold de la Torre in Contempt
“Dr. Ralph de la Torre is not above the law.”
That’s what U.S. Senator Bernie Sanders (Ind-Vt.) said at the outset of a September 19 meeting of the Senate’s Committee on Health, Education, Labor, and Pensions (HELP) that Sanders chairs.
The committee voted unanimously (20-0) on two resolutions to begin the process of holding de la Torre, the CEO of the bankrupt Steward Health Care system, in contempt for failing to honor a HELP subpoena to testify last week.
One resolution instructs Senate Legal Counsel to bring a civil suit in the District Court for the District of Columbia to require de la Torre’s compliance with the subpoena and his testimony before the HELP Committee. Another criminal contempt resolution refers the matter to the U.S. Attorney for the District of Columbia to criminally prosecute de la Torre for failing to comply with the subpoena.
Both resolutions must first go to the full U.S. Senate for a vote.
De la Torre has argued that he can’t testify while the bankruptcy proceedings are still underway in Texas, and because Steward has formed a special internal committee, of which he is not a part, to handle all bankruptcy issues. The Senate HELP committee said it reviewed his objections and did not find them compelling.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association