Hospitals Put in “Impossible Position”

INSIDE THE ISSUE
> Hospitals Bear Burdens
> $1 Billion to Community Health
> 1,792 Stuck Patients
> MHA’s Workforce Summit
> Legislative Update
> Transition
MONDAY REPORT
The “Hospital Dollar” is Evaporating Quickly
After the quality of care delivered, the biggest emphasis in healthcare – from those delivering it, to those receiving and paying for it – is its cost.
Rising healthcare costs cut into household incomes and are borne by employers and taxpayers. Healthcare providers, a major component of each “healthcare dollar” spent, are frequently in the crosshairs in debates over cost, even as hospitals – especially those in Massachusetts – continue to deliver some of the finest, lifesaving and life-improving care on the globe.
But while much of the focus remains on healthcare’s overall cost to society, less attention is placed on some of the biggest underlying factors: the incremental, ever-growing costs hospitals themselves are asked to absorb just to keep the entire healthcare system afloat.
For example, when this fiscal year draws to a close in October 2024, Massachusetts hospitals are expected to shoulder approximately $210 million in unreimbursed costs to care for the uninsured and underinsured patients in the state. Every year, hospitals and health insurance companies each contribute $165 million to the Health Safety Net to care for the uninsured but each year the fund runs short – by an estimated $210 million in FY24 and $220 million in FY25. Hospitals alone – without assistance from insurers or the state – must cover the shortfalls.
Or take the $400 million per year in unreimbursed care for the thousands of patients each month that are stuck in hospitals unable to transfer to the next level of care (see story below). Longer stays do not translate into larger revenues. Hospitals receive a relatively fixed cost from insurers for such patients no matter how long they occupy a hospital bed, meaning they must absorb the costs of this extra care on their own.
MHA along with other healthcare groups have detailed as much as $1.75 billion in annual cost waste due to unnecessary insurance administrative burdens that result in wasted resources expended while attempting to reconcile denied claims; excessive time spent contesting claims denials; and claims processing delays.
In an effort to reduce costs and improve patient access, hospitals are investing in telehealth systems, mobile integrated health, and hospital-at-home programs that deliver inpatient level care outside of the hospital’s walls. They’re purchasing (or renting) properties and outfitting them to deliver urgent care outside of emergency departments. Yet all of these innovative care delivery models require immense investments – which again are not reimbursed by the government or by the private health insurance industry.
Evidence of the continued financial pummeling of hospitals was released last Thursday by the state’s Center for Health Information and Analysis in its quarterly report on the health of Massachusetts hospitals and health systems. That report found that through March 2024, the statewide median operating margin of hospitals was negative 0.1%. Fifty percent of hospitals (30) reported negative operating margins. Sixteen of 22 hospital health systems (73%) experienced negative operating margins. That means, simply and of great concern, that the great majority of hospitals and their physician practices are expending more money to care for patients than they are taking in.
“CHIA’s latest report should serve as an enormous red flag on the state of hospital finances in Massachusetts, which have only worsened after four-plus years of unrelenting cost pressures,” said MHA’s Senior Vice President, Healthcare Finance & Policy Dan McHale. “The growing list of financial burdens now being funneled toward providers is of serious concern. One by one, they are adding up and putting our providers in an impossible position to recover.”
In addition to the factors described above, McHale noted that the state budget now being finalized assumes the Healey Administration’s plan of $300 million in MassHealth payment reductions. The Executive Office of Health and Human Services indicated that the hospital portion of those cuts could reach $100 million. Coordinated attacks on the 340B drug pricing program, which hospitals rely on for investments in their communities, are also destabilizing the healthcare system.
“Hospitals are paying the price to keep the system afloat, and these factors must be addressed through collaborative public policy and assistance from other components of the healthcare community,” McHale said. He also noted that the health insurance industry, whose main task is coordinating the paperwork component of the healthcare system, has significant reserves over and above the minimums the state requires them to possess; such reserves have not yet been redirected to help support patient care.
“It will take everyone – providers, insurers, government partners, and beyond – to embrace bold solutions, set our local hospitals on a definitive road to recovery, and keep care accessible for the millions of patients across the commonwealth,” McHale said.
A First: Massachusetts Hospitals’ Community Benefits Eclipse $1 Billion
For the first time, Massachusetts hospitals’ community benefits investments topped $1 billion over the course of a single fiscal year. The findings, which cover community funding for FY2023, were recently released by Attorney General Andrea Campbell.
Massachusetts hospitals are renowned for the lifesaving, compassionate care they deliver each day for patients and families. What receives less attention, but is of vital importance to public health, are the activities they fund outside their walls to support people’s wellbeing.
These investments – known as “community benefits” programs – address specific health concerns and disparities identified in collaboration with trusted local partners, ranging from faith-based organizations to schools, first responders, and advocacy groups. Programs are provided at no cost to the populations being served and are not reimbursed by government entities or insurance companies.
In fiscal year 2023, local hospitals devoted $1.03 billion to local community benefits programs – a 14% increase from FY22. These investments continued to grow even as the hospital community struggled with severe financial losses and well-documented financial instability – pressures that still persist today (see stories above).
“Community-based programs are a central aspect of fostering health and wellbeing, particularly for those with mental and behavioral health concerns,” said Attorney General Andrea Joy Campbell. “My office and I will continue to spotlight the critical investments of our hospitals and HMOs, which help expand health access and equity and meaningfully address the needs of communities across the commonwealth.”
Community benefit programs are seen in public schools and senior centers. They permeate neighborhoods in mobile health vans and farmer’s markets, through job fairs and health screenings, and in programs that address substance use disorder, violence prevention, and LGBTQ rights. As the hospital-funded programs lift up one section of society, their positive results reverberate throughout entire communities and affect generations. For example, hospital-based outreach to improve housing quality can reduce asthma rates in children, which improves school scores, which lowers hospital admissions and healthcare costs – and so on.
Hospitals detail their specific community outreach efforts in annual reports to the Massachusetts Office of the Attorney General in addition to submitting information to the Internal Revenue Service as required by the Affordable Care Act. Examples of hospital-specific programs can be accessed through the Attorney General’s webpage.
“There isn’t another economic sector that steps up for its communities more than our local hospitals, especially under the most challenging of circumstances,” said Steve Walsh, MHA’s president and CEO. “These investments embody our hospitals’ commitment to leading on community-based health, closing pervasive disparities, and being a part of their patients’ everyday lives. We are grateful for Attorney General Campbell’s guidance through every step of this process as we continue to address the real-time needs of people in every neighborhood of the commonwealth.”
Hospitals’ community benefit investments are separate and distinct from their $165 million annual investment in the Health Safety Net fund, which covers care for uninsured and underinsured patients in Massachusetts. Hospitals and health insurance companies pay an equal amount to fund the Health Safety Net, but hospitals are solely responsible for any funding shortfall. The Health Safety Net shortfall is expected to exceed $210 million in FY2024.
Hospitals will be filing their FY2024 community benefits report in spring of 2025.
Another Sobering Month of Patient Transition Challenges
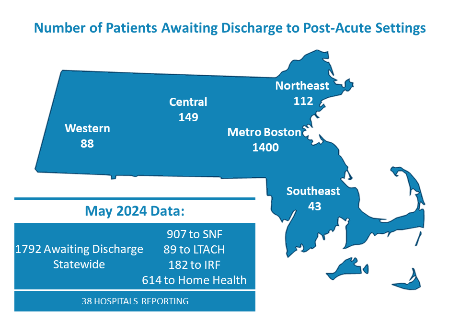
The data doesn’t lie: Massachusetts acute care hospitals consistently have nearly 1,800 patients stuck in beds unable to transition to the next level of care – whether it be at a rehabilitation facility or home care.
MHA surveys its member hospitals each month and the latest data – from May, and from just 38 hospitals – shows 1,792 patients awaiting discharge; 907 are awaiting a bed in a skilled nursing facility, 89 are waiting for an opening at a long-term acute care hospital, 182 to an inpatient rehabilitation facility, and 614 are awaiting home healthcare services. The “good” news is that there were 182 fewer patients stuck in May than there were in April.
The reasons for the backups are also well documented; workforce shortages at the post-acute care facilities means that even if a bed is available there isn’t a worker to staff it. Delays in getting prior authorization approvals from health insurance companies, especially the national insurers, is a major factor in patient transitions. If a patient is unable to make a care decision for themselves, or does not have someone designated to do so for them, a hospital must then go through the courts to designate a guardian – which can take months. Also, many patients with cognitive or other impairments are unable to fill out a MassHealth application to receive long-term care benefits. This requires intervention by the courts – known as a conservatorship – that further delays the process. (Honoring Choices Massachusetts has created a webpage with information, downloadable tools, and links to help people through the complicated guardianship process.)
Patient care is obviously affected by the inability to move the patient to the right care setting. But there is a financial cost as well; insurance companies typically pay hospitals a fixed amount per-patient, per-diagnosis. If a patient is stuck in a hospital for additional days after their course of care has been completed, the hospital generally does not receive any additional funding and often must absorb the additional costs on its own. MHA has estimated this cost to hospitals totals more than $400 million annually. Plus the occupied bed cannot be used to help ease overcrowding in a hospital’s emergency department.
MHA’s Workforce Summit

MHA’s Annual Workforce Summit last Thursday drew nearly 150 attendees at the association’s headquarters in Burlington, Mass. The summit featured panels and breakout sessions detailing the latest innovations in attracting and retaining workers in a time of increasing workforce vacancies and ongoing pressures. Secretary Lauren Jones of the Executive Office of Labor and Workforce Development delivered the keynote address. She said, “In this tight labor market, we have to think differently. We also have to be very intentional with how we reduce barriers to employment, how we reimagine, how we bring in talent to our workforces, and how we create more intentionality to create the results that we all need.”
Healthcare Bill Due; Shield Bill Passed
The State Senate’s healthcare reform bill could be released as early as today.
The bill, drafted in response to the House’s oversight bill (H.4643, An Act enhancing the market review process) that passed in May, is expected to be on a very tight schedule for amendment submissions, debate, and ultimate vote. The rapid schedule is necessary if the House and Senate are to work out compromise legislation by the end of the legislative session on July 31.
Last week, the House unanimously passed H.4844, An Act providing protections for reproductive or gender-affirming care location information, which prohibits cell phone carriers and other companies from collecting or selling locater information on people seeking reproductive and gender-affirming healthcare. After the U.S. Supreme Court’s Dobbs decision, many states are not only prohibiting abortion but attempting to make it illegal for people to seek abortion services in other states. Similar restrictions are being imposed on gender affirming care.
H.4844 protects such patients travelling to Massachusetts, as well as Bay State residents and even providers from harassment and/or legal consequences for seeking/providing care.
The House passed the bill unanimously. It is unclear if the Senate will pass a similar measure before July 31.
Transition
Berkshire Health System announced that Anthony Scibelli will lead the system’s 25-bed Fairview Hospital in Great Barrington under the title of system vice president and chief operating officer. Scibelli is currently vice president of operations and chief administrative officer at Cooley Dickinson Hospital, which is part of the Mass General Brigham system. He will begin his role at Fairview in September. Scibelli has a B.A. from Worcester State College, an M.A. from Lesley University, and an MBA from SUNY Albany.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association