Focus on PBMs, Healey at Annual Meeting, and more …

INSIDE THE ISSUE
> FTC Slams PBMs
> Long-Term Care Task Force
> 1,880 Stuck Patients
> Prior Auth Guidance
> Governor Delivers State of the State
> Telehealth and OUD
> MLK Jr. Day
MONDAY REPORT
Focus, and Criticism, Directed Towards PBMs
The Federal Trade Commission (FTC) last week issued its second scathing report in the past six months on pharmacy benefit managers (PBMs), the entities that negotiate with drug manufacturers on behalf of employers and health insurance companies, help create lists of medications (known as formularies) covered by insurance, and reimburse pharmacies for prescriptions.
The three largest PBMs are Optum and Express Scripts, owned by the large national insurance companies UnitedHealth Group and Cigna, respectively, and CVS Health’s CVS Caremark.
The FTC report found that the big three PBMs marked up numerous specialty generic drugs dispensed at their affiliated pharmacies by thousands of percent, and many others by hundreds of percent. These markups allowed the PBMs to generate more than $7.3 billion in revenue over and above the National Average Drug Acquisition Cost (NADAC) from 2017 to 2022, according to the FTC report.
While the PBMs profited, the cost of drugs to patients, employers, and providers have increased dramatically. According to the Health Policy Commission (HPC), the consistently largest percentage growth in healthcare spending in Massachusetts in recent years has been attributable to drug costs.
“Pharmaceutical spending has been a major driver of healthcare spending [in Massachusetts] in recent years,” the HPC’s Executive Director David Seltz said at the commission’s board meeting last Thursday. “Pharmacy spending for commercial enrollees grew 8.2% per year from 2019 to 2022 and contributed meaningfully to our state’s overall spending growth.” Seltz said if pharmacy spending adhered to the state’s 3.1% cost growth benchmark during those years, total spending growth would have been 4.1% as opposed to the 5.8% Massachusetts experienced in 2022 – the most recent cost trend data.
The FTC report found that nationally the big PBMs were steering the prescriptions that it marked up by thousands of dollars to the pharmacies that their parent companies owned. In general, according to the FTC, the PBMs paid their pharmacies more than unaffiliated pharmacies for almost every drug.
“Spread pricing” by the big three PBMs also accounted for another $1.4 billion in income to them, the FTC said. Such pricing occurs when the PBM bills their plan clients more than they reimburse pharmacies for the drugs and pocket the difference.
In the recent healthcare oversight and pharmacy bills that Governor Maura Healey signed into law this month, state regulators are granted more authority to oversee PBMs. The HPC will create a new Office of Pharmaceutical Policy & Analysis, and the state’s Center of Health Information & Analysis is empowered to collect new data from the PBMs.
Most significantly, the Division of Insurance (DOI) is given authority to regulate and license PBMs operating in the state. The rulemaking to implement the law could include the authority for DOI to conduct audits of PBMs. This Thursday, January 23, from 1 to 3 p.m., DOI will hold a discussion on pharmacy benefit managers as part of its information sessions to examine cost drivers underlying the healthcare premium environment.
TACPAC Must Deliver Long-Term Care Report by July 31
The state’s new Transitions from Acute Care to Post-Acute Care (TACPAC) Task Force held its inaugural meeting last Wednesday, initiating a seven-month process, the end of which will culminate in a report to the Massachusetts legislature by July 31.
TACPAC was established through the October 2024 enactment of An Act to Improve Quality and Oversight of Long-Term Care. That law puts in place a number of tools to address barriers to post-acute care, including expedited prior authorization for post-acute care services (see story below), MassHealth reimbursement rate add-ons for specialized care for underserved populations, and creation of the task force. The law also strengthens the commonwealth’s oversight of nursing homes, provides anti-discrimination protections for LGBTQ+ nursing home residents, and permanently allows assisted living residences to offer basic health services.
Assistant Undersecretary of Health & Human Services Joanne Marqusee chairs the 17-member group; MHA’s Senior Director, Virtual Care & Clinical Affairs, Adam Delmolino, serves as MHA’s task force representative.
Last Wednesday’s meeting was primarily an introductory/organizational gathering. Future meetings will examine a variety of steps to ease transitions, from easing insurance companies’ administrative barriers to discharge, to post-acute capacity challenges, to the need for increasing public awareness of healthcare proxies and the importance of designating a healthcare agent.
Care transitions from acute care to post-acute care are a persistent problem in the Massachusetts healthcare system, resulting in thousands of patients being stuck in hospitals, ED boarding, and rising healthcare costs (see story below).
Last Monthly Survey Shows 1,880 Stuck in Hospitals
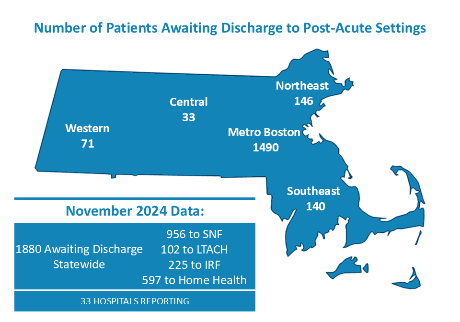
MHA’s monthly survey of hospitals shows that at a point in time in November 2024, the latest survey, 1,880 patients were stuck in Massachusetts acute care hospitals, unable to be transferred to either a skilled nursing facility, long-term acute care hospital, inpatient rehabilitation facility, or home healthcare.
During 2024, the number of patients unable to transfer exceeded 2,000 for the first time in the three-year survey history and persistently hovered above the 1,500 mark. As has been reported, if a patient is stuck in a hospital after their normal course of care has been completed, the patient cannot access the specialty care they need. At the same time, the hospital does not get paid for the additional stay and must often absorb the costs of keeping the patients in an inpatient bed. MHA has estimated this cost to hospitals totals more than $400 million annually. Plus the occupied bed cannot be used to help ease overcrowding in a hospital’s emergency department. Patients and their families suffer from the delays.
Policymakers have recognized the importance of resolving the issue, which led to passage of the recent long-term care act, and creation of a task force to investigate the issue (see story above).
Expedited Prior Auth Now in Place for Discharge to Post-Acutes
As part of the passage of the new Act to Improve Quality and Oversight of Long-Term Care (see story above), a two-year pilot program is in place requiring insurers in the Group Insurance Commission and MassHealth, along with Massachusetts-licensed commercial plans to make a determination, in one business day, whether to approve or deny a prior authorization request to discharge an acute hospital inpatient to a post-acute care facility or home care service.
If a calendar day following the submission of a prior auth request is not a business day (say, a weekend or holiday), and the post-acute care facilities or services will accept the patient, then prior authorization will be waived for that patient’s care.
Under the provisions of the law, both the state’s Division of Insurance and MassHealth are required to issue sub-regulatory guidance to effectuate this new program. So far, MassHealth has issued guidance only for expedited prior auth for discharges to home care services. Given the capacity constraints that hospitals are enduring today, there is much anticipation around additional guidance from DOI and MassHealth.
In State of the State, Healey Focuses on Primary Care
Governor Healey last Thursday delivered an upbeat State of the State speech, her second, in the State House chamber, detailing achievements from 2024 and stressing the need to make Massachusetts more affordable going forward.
“State revenues are growing. But the cost of providing services has gone up; and federal pandemic relief is long gone,” Healey said. “So, we will continue to control spending and live within our means just as every family and business is doing. So, I promise: the budget I submit next week will prioritize efficiency, action, and impact. We need every dollar to make a difference. I want to make things move and go in our state.”
On the healthcare front, the governor reflected on the 31 new community behavioral health centers across Massachusetts, which have been credited for easing emergency department boarding and addressing the youth mental health crisis. She said more needs to be done and that her budget will fund behavioral health support in schools to bring care closer to students. She also decried the lack of primary care physicians in the state and the resultant long wait for doctor’s appointments.
“I am directing my Administration to shift healthcare resources to the front lines,” she said. “And by that, I mean primary care. We’ll drive career training pipelines to grow the workforce. I want a whole army of primary care providers out there, so when you call for an appointment, you’ll get one.”
Telehealth Rules Allows Controlled Substance Prescriptions
Last week, the Drug Enforcement Administration (DEA) released a proposed rule that would create a “Special Registration” framework for DEA-registered practitioners to engage in telemedicine and prescribe controlled substances. There would be various tiers of registration based on the schedule of drugs being prescribed, and much heightened recordkeeping and reporting requirements than currently exist.
Also last week, the DEA with the Department of Health and Human Services released a final rule expanding the ability of DEA-authorized practitioners to prescribe via telemedicine schedule III-V controlled substances like buprenorphine approved by the FDA for the treatment of opioid use disorder. This includes audio-only telemedicine encounters if there has been no in-person evaluation between the practitioner and the patient. The final rule should be effective on February 16, 2025.
MHA’s Offices Closed in Honor of MLK Jr. Day
MHA’s offices are closed today in recognition of Martin Luther King Jr. Day. Today, we reflect on the legacy of Dr. King, whose enduring vision inspires MHA’s work to advance health equity, promote health justice, and eliminate systemic barriers to the high-quality care every patient deserves.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association