CDC Cuts, HHS Reorg

INSIDE THE ISSUE
> CDC Terminates Awards
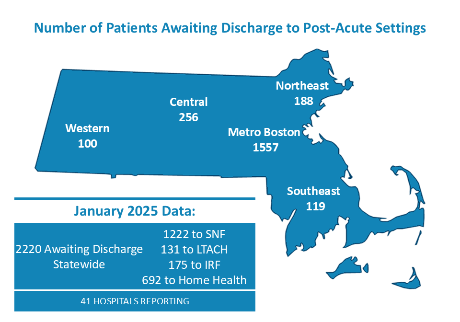
> 2,220 Stuck Patients
> HHS Cuts
> Fleishman, Coburn Join MLSC Board
MONDAY REPORT
Public Health Programs Dealt a Blow
The Centers for Disease Control and Prevention (CDC) last week informed public health groups across the U.S. that it was clawing back $11 billion in public health infrastructure grants. According to the Healey Administration, Massachusetts is expected to lose $100 million from the cuts. Also, the state’s Department of Mental Health is expected to lose federal funding after the Substance Abuse and Mental Health Services Administration also terminated awards.
According to the state, the CDC funding supports the state’s public health laboratory, including treatment and testing for respiratory diseases such as bird flu. “Much of the funding goes directly to the community, including to community health centers across the state to support workforce and community investments,” the governor’s office wrote.
In announcing the grant termination notices, U.S. Health & Human Services noted that the grants were originally created during the height of the COVID-19 pandemic. “The COVID-19 pandemic is over, and HHS will no longer waste billions of taxpayer dollars responding to a non-existent pandemic that Americans moved on from years ago,” the department wrote.
“This decision by the Trump Administration is troubling and potentially devastating to public health,” said Dr. Robbie Goldstein, commissioner of the Massachusetts Department of Public Health. “We rely on these funds to carry out important work at the Department and with our partners in the community … They represent investments in the core functions of public health. We are working quickly to analyze the fiscal and operational impacts of these abrupt terminations.”
Last Wednesday, Goldstein testified at an informational hearing before legislature’s Joint Committee on Public Health. He told the committee that of DPH’s estimated $1.75 billion budget, approximately $700 million comes from the federal government across many agencies, including not only the CDC, but also the Environmental Protection Agency, and Department of Housing and Urban Development, among others.
Ongoing Work to Resolve the Stuck Patient Issue
The hospital “throughput” problem – that is, the failure to move patients efficiently through the healthcare system, from one level of care to the next – appears to be worsening, according to the most recent survey of hospitals.
Survey data shows that hospitals surveyed in January reported 2,220 stuck patients, unable to transition from acute care hospitals to the next level of care in either a skilled nursing facility, long-term acute care hospital, inpatient rehabilitation facility, or home health services. The November 2024 total of stuck patients was 1,880; December’s total was 1,995.
Resolving the worsening problem will require a series of steps, which include increasing the supply of healthcare workers needed to staff licensed beds in post-acute facilities; compelling insurers to be available 24/7 so that they can authorize transfer requests; and ensuring that patients have healthcare proxies, care directives, and other alternatives to guardianship and conservatorship on file so their wishes can be carried out promptly if they are incapacitated – without involving the courts. Efforts are underway on each of these fronts but the inability to transfer patients out of hospitals and free up care beds for patients waiting in hospital emergency departments remains a serious issue.
A recent KFF News story highlighted SNF (Skilled Nursing Facility) at Home” models from UMass Memorial Health and Mass General Brigham, which have shown growing promise in recent years. Such programs typically lack the insurance supports to grow at-scale, however.
“SNF at home programs are viewed as a potential solution to the shortage of nursing home and rehab beds that are contributing to the significant throughput challenges in our healthcare system,” State Rep. Thomas Stanley (D-Waltham) wrote in a LinkedIn post last Friday in reaction to the story. “With Massachusetts Health & Hospital Association estimating approximately 1,995 patients awaiting hospital discharge in December 2024, we certainly need to utilize all the tools at our disposal to ensure patients are receiving the care they need without any unnecessary delays.”
Stanley is a leading sponsor of MHA-backed legislation An Act Improving Access to Post-Acute Services (H.1412/S.903), which aims to streamline healthcare transitions, enhance support for post-acute care, improve patient protections, and strengthen the long-term care system in the commonwealth. Senator Pavel Payano is the leading Senate sponsor of the legislation.
U.S. HHS to Cut Another 10,000 Workers & Reorganize
U.S. Health & Human Services (HHS) announced last week that it would cut 10,000 workers. Added to the roughly 10,000 that already have taken early retirement and buyouts, HHS’ workforce will be reduced to 62,000 from 82,000.
According to an HHS fact sheet, the Food and Drug Administration will lose 3,500 workers, the Centers for Disease Control and Prevention (CDC) will see a 2,400 worker reduction, National Institutes for Health (NIH) will cut 1,200 workers, and Centers for Medicare and Medicaid Services will cut its workforce by 300.
Regional HHS offices will be cut from 10 to five, with the Boston office being one of the ones closed.
According to HHS, the current 28 divisions within HHS will be consolidated into 15 new divisions, including the new “Administration for a Healthy America” (AHA).
“The overhaul will implement the new HHS priority of ending America’s epidemic of chronic illness by focusing on safe, wholesome food, clean water, and the elimination of environmental toxins,” HHS wrote in a media release.
Specifically, the new Administration for a Healthy America will combine within it the Office of the Assistant Secretary for Health (OASH), Health Resources and Services Administration (HRSA), Substance Abuse and Mental Health Services Administration (SAMHSA), Agency for Toxic Substances and Disease Registry (ATSDR), and National Institute for Occupational Safety and Health (NIOSH).
The Administration for Strategic Preparedness and Response (ASPR) will now be within the CDC.
HHS will create a new Assistant Secretary for Enforcement to oversee the Departmental Appeals Board (DAB), Office of Medicare Hearings and Appeals (OMHA), and Office for Civil Rights (OCR) “to combat waste, fraud, and abuse in federal health programs.”
HHS will merge the Assistant Secretary for Planning and Evaluation (ASPE) with the Agency for Healthcare Research and Quality (AHRQ) to create the Office of Strategy to enhance research. And the Administration for Community Living (ACL) that oversees programs that support older adults and people with disabilities will be integrated into other HHS agencies, including the Administration for Children and Families (ACF), ASPE, and CMS.
Fleishman, Coburn Named to Mass. Life Sciences Center Board
The Healey Administration has appointed MHA’s Executive Vice President and Chief Innovation Officer Valerie Fleishman, as well as Mass General Brigham Chief Innovation Officer Chris Coburn, to the Massachusetts Life Sciences Center (MLSC) Board of Directors.
The MLSC is an economic development investment agency that supports life sciences in Massachusetts through public-private funding initiatives.
Last year’s passage of the Mass Leads Act economic development bill created new seats on the MLSC board to represent medtech, healthcare, digital health, and health equity.
Among her duties at MHA, Fleishman leads strategic initiatives, innovation advancement, and new business development. Prior to joining MHA, Fleishman served as executive director of the Network for Excellence in Health Innovation (NEHI), the national non-profit.
Also appointed to the MLSC last week were Brian Johnson, the president of the Massachusetts Medical Device Industry Council; and Dana Mendenhall, senior vice president and global head of commercial and portfolio strategy for the plasma derived therapies business unit at Takeda.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association