Budget Debate Begins; Debt Talks & Medicare

INSIDE THE ISSUE
> The Senate Budget Debate
> The Debt Limit Talks
> Flexibilities Extended
> Reporting Reduction
> DSH Cuts Looming
> MOLST to POLST
> Transition
MONDAY REPORT
Massachusetts Senate Budget Debate Begins
The Massachusetts State Senate begins its debate on its $55.85 billion Fiscal Year 2024 state budget and the 1,049 amendments to it that were filed last week.
MHA’s priority amendments on the behavioral health front (Amendments 542 and 543) were both filed by Sen. John Keenan (D-Quincy). One seeks to ensure that hospital EDs get compensated for providing crisis evaluations to uninsured and Medicare-only behavioral health patients. Such evaluations were previously provided by emergency service programs, but the ABC Act (Chapter 177 of the Acts of 2022) shifted that responsibility to EDs; however, the funding and coverage requirements were never changed, leaving hospitals at risk. Amendment 543 would extend Chapter 177’s required commercial coverage of behavioral health crisis services, including ED-based crisis evaluations, and youth community crisis stabilization services, which are a key piece of the Roadmap for Behavioral Health Reform, and which had not been implemented at the time of Chapter 177’s passage.
Three priority amendments (416, 418, and 525, filed by Senators Barry Finegold (D-Andover), Brendan Crighton (D-Lynn), and John Cronin (D-Leominster), respectively) address workforce issues by providing one-time grants to support Boston MedFlight and hospital-based emergency medical services providers (416); adding $250,000 to a DPH line item to fund a pipeline program to create partnerships between community colleges and hospitals to recruit mental health workers (418); and addressing access to vaccinations by expanding the types of physicians and advanced practice providers that can delegate the administration of an immunization to a certified medical assistant.
A telehealth amendment (417) filed by Sen. Finegold would restore primary care and chronic disease telehealth rate parity to 100% of in-person service for two years. This would revive a COVID-19 era policy, align with Medicare policy, and follow the recent recommendation from the state’s Health Policy Commission. Another telehealth amendment (554), from Sen. Jake Oliveira (D-Ludlow), would establish task forces to explore alternative licensure-reciprocity models, including a regional approach, to allow Massachusetts-licensed caregivers to provide continuous care by telehealth to their established patients across state lines.
Federal Debt Breach Could Affect Medicare and Medicaid Payments
Congressional leaders and President Biden have been negotiating an agreement for weeks on how to address the current debt limit, which is set to expire in June. The federal debt limit is the total amount of money that the U.S. government is authorized to borrow to meet it existing legal obligations, including Social Security and Medicare benefits, military salaries, tax refunds, and other payments. If the debt limit expires, the Treasury Department will have to make some very difficult decisions about how to allocate limited resources across the federal government; like all other federal payments, Medicare and Medicaid would be subject to delays or reductions if the Treasury ran out of cash and borrowing room.
Treasury Secretary Janet Yellen sent a letter on Monday to House Speaker Kevin McCarthy stating that the debt ceiling will be breached by “early June, potentially as early as June 1.” Congress has always acted to raise the debt limit and has done so 78 times under presidents and congressional leadership from both parties.
CMS Extends Telehealth Billing for Hospital-Employed Clinicians
On May 12 the Centers for Medicare and Medicaid Services (CMS) updated its COVID flexibilities FAQ to clarify that hospital-employed clinicians can continue to bill Medicare for telehealth services through the end of calendar year 2023. This clarification addresses telehealth billing for hospital-employed physical therapists, occupational therapists, speech language pathologists, diabetes self-management training, and medical nutrition therapy providers. Originally CMS had indicated that billing for these telehealth services would end when the public health emergency ended May 11.
Additionally, CMS published guidelines allowing virtual supervision of residents through December 31, 2023. The move allows teaching physicians in all teaching settings to be present virtually, through audio/video real-time communications technology, for purposes of billing under the Medicare Physician Fee Schedule for services they furnish involving resident physicians.
DPH Ends Some, not All, COVID-19 Reporting
Two years ago, on May 25, 2021, Massachusetts Department of Public Health (DPH) issued a directive to providers advising them to report any hospitalizations or deaths attributable to COVID-19 vaccine breakthroughs – that is, an event that occurred at least 14 days after the final dose of COVID-19 vaccine. Last week, DPH ended that reporting requirement.
According to the state’s COVID-19 Interactive Data Dashboard, on January 2, 2023, there were 1,282 patients hospitalized in Massachusetts due to COVID-19 and of those, 842 were fully vaccinated. On May 9, there were 174 hospitalized patients, of which 109 were fully vaccinated.
DPH last week also issued a notice reminding all hospitals that they must continue to report state and federally required COVID-19-related data to DPH. This sheet shows the 100-plus data elements still required to be reported.
Bipartisan Letter Seeks to Forestall DSH Cuts
A bipartisan letter to U.S. House Speaker Kevin McCarthy (R-Calif.) and Democratic Leader Hakeem Jeffries (N.Y.) decrying $8 billion in annual cuts to disproportionate care hospitals (DSH) was signed by 231 members of Congress, including seven from the Massachusetts House delegation.
The cuts to the DSH are mandated by the Affordable Care Act which reasoned that as previously uninsured and underinsured people got coverage under the ACA, uncompensated care costs to hospitals would drop and the DSH payments could as well. But the uninsured problem across the U.S. persists and the DSH continue to operate on very thin margins. With Medicaid redeterminations now occurring as many pandemic-era eligibility protections are ending, many individuals are expected to temporarily lose coverage, causing uncompensated care costs to spike and putting more pressure on the DSH.
“Since 2013, Congress has recognized the critical need for Medicaid DSH payments by passing thirteen pieces of legislation delaying what would have been immediate cuts to the program,” reads the bipartisan letter spearheaded by Rep. Yvette D. Clarke (D-N.Y.) “On October 1st, safety net hospitals will face an $8 billion annual cut that is equivalent to more than two-thirds of annual federal DSH spending. These cuts would continue apace through FY2027 … Our nation’s rural and urban safety net hospitals cannot sustain losses of this magnitude, leaving our constituents and communities without access to the medical care they depend on and need.”
The letter signees call for passage of H.R. 2665, the Supporting Safety Net Hospitals Act, which would eliminate the cuts for FY24 and FY25 entirely. Among those signing the letter were Massachusetts Democrats Jake Auchincloss, Bill Keating, Lori Trahan, Seth Moulton, Stephen Lynch, Ayanna Pressley, and James McGovern.
The Document That Tells EMTs What Care You Want
Massachusetts is changing the document that patients use to detail their care preferences to the emergency healthcare professionals who are treating them during a medical crisis or when patients cannot speak for themselves.
The new Portable Orders for Life Sustaining Treatment (POLST) form will eventually replace the current MOLST form, or Medical Orders for Life Sustaining Treatment, which is printed on pink paper. POLST forms will be filed electronically, making them more easily visible across care settings, and less likely to get lost. POLST will also be able to be used across state lines.
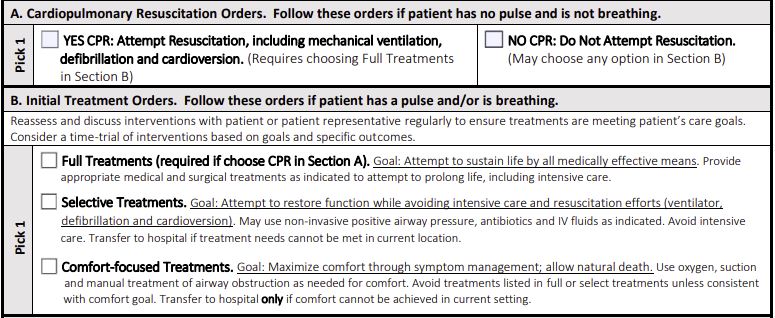
The forms detail whether a patient wants CPR to resuscitate them and whether they are accepting or refusing medical treatments, including those that might extend life. A POLST form is a medical order, like a prescription. An advance directive is an entirely different and legal document that tells who the patient wants making medical treatment decisions for him/her when he/she cannot speak and gives general directions on treatments.
The MOLST-to-POLST transition will be in pilot test mode at Fairview Hospital and Cooley Dickinson Hospital beginning in June. In the Spring/Summer 2024, the state will test the ePOLST registry and begin drafting regulations in the hopes of beginning POLST implementation towards the end of 2024. In the interim, all POLST forms are valid and must be honored just as a MOLST form would be.
Transition
Michael Gustafson, M.D., the president of UMass Memorial Medical Center for the past five years, MHA Board member, and chair of the Board’s Clinical Issues Advisory Council, has decided to step down from leading the hospital, effective July 28. A system wide e-mail announcing his departure said that Gustafson “intends to pursue his passion for improving quality of care and patient safety, the patient-family experience, and clinical innovation on a regional and national level, expanding upon his 27 years of experience in these areas as a healthcare leader in Massachusetts.” Justin Precourt, R.N., the chief nursing officer for the Medical Center and chief nurse executive for UMass Memorial Health will serve as interim president. Gustafson’s involvement with MHA over the years directly influenced much of the association’s advocacy and work around improving patient and workforce safety, advancing equity, and, most recently, addressing the pandemic.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association