Benchmark: Looking Back to Plan for the Future

INSIDE THE ISSUE
> The Benchmark: Rewind to ’23
> The Benchmark Process
> The FY26 Budget
> EO Setbacks in the Courts
> Fletcher “Flash” Wiley
MONDAY REPORT
HPC Looks Back to Plan for Uncertain Future
The Health Policy Commission this Thursday holds its annual hearing on the state’s healthcare cost growth benchmark – the targeted rate of growth for total healthcare expenditures (THCE) in Massachusetts.
To set the benchmark for calendar year 2026, the HPC on Thursday will assess THCE and other data from 2022-2023. (THCE is the per capita measure of all healthcare spending in the commonwealth.) Using two-year old data to set a benchmark for the coming year is customary practice for the HPC.
The current benchmark sits at 3.6%, a vestige of what the state imagined as an achievable goal under normal economic circumstances more than a decade ago. However, cost growth for 2022-2023 is expected to significantly exceed that factor due to persistent, well-documented financial challenges that were roiling the sector two years ago – and which still exist today. MHA has long argued that this approach to the benchmark has outlived its ability to align with the state’s overall economic growth, especially in recent years.
The two-year lag means current or past inflation trends, a global pandemic, or the rapidly changing labor or pharmaceutical sectors, among other factors, can play an outsized role in how the system performs compared to the pre-set benchmark. For example, a two-year retrospective look misses last year’s destabilizing Steward Health Care bankruptcy. And the coming year’s benchmark, under which all hospitals and health systems will operate, is unable to factor in any significant future events, such as increased supply costs due to tariffs, potential Medicaid cuts, continued workforce shortages, and more.
“Looking back, 2023 was a deeply challenging year for our local healthcare providers, and we expect the state’s numbers will show the steep costs of keeping the system afloat for patients,” said MHA’s Executive Vice President and General Counsel Mike Sroczynski. “That is why the current benchmark process, while well-meaning, is somewhat divorced from reality. As we have seen over the past five years, the data foundation on which the benchmark is built – from potential gross state product to expenditures from years ago – is a fragile foundation at best. And equally concerning is the fact that there seems to be little recognition that the healthcare sector is not separate and apart from the economy as a whole.”
The 2022-2023 base year that will inform the 2026 benchmark-setting process was one of the worst for the hospital community. While hospital spending almost certainly grew to keep up with cost demands, those same organizations’ financial health remained perilous. The statewide acute hospital median operating margin in hospital fiscal year 2022 was negative 1.3%. In 2023, the operating margin “improved” to just 0.2%. In FY2023, hospitals were still paying approximately $1.5 billion annually for contract labor, similar to the unsustainable cost trend experienced in FY2022.
Noting that “healthcare does not happen in a vacuum,” Sroczynski added, “It is subject to the same economic forces and pressures as every other sector – especially in recent years, when the cost for every service and good has spiked dramatically. But unlike other segments of the economy, hospitals cannot simply pass along rising costs to consumers or make wholesale changes to their product lines. They maintain staffing and services 24/7/365, regardless of economy, weather, workforce vacancies, supply shortages, inflation, or the tail end of a devastating pandemic.”
MHA has consistently advocated for bringing all parties “back to the table” to revisit the benchmark process, from its outdated reliance on potential gross state product to the timeliness of data used to reach decisions (see story below).
How the Benchmark is – and Isn’t – Developed
The intent of state’s 2012 cost containment law was to tie healthcare growth to overall state economic growth. However, for the past ten years, the commonwealth has not linked the benchmark to Massachusetts economic activity. Instead, the state has measured healthcare spending to a stagnant growth rate of 3.6% that is set arbitrarily each year.
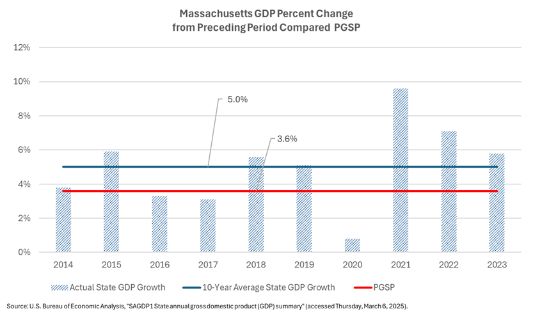
Unless the Health Policy Commission Board recommends an alternative cost growth benchmark that is approved by the legislature, the annual benchmark is equal to the growth rate of the potential gross state product (PGSP). PGSP – that is, the measure of the commonwealth’s long-term economic growth at full employment – is determined each year after the Secretary of Administration and Finance and the House and Senate Chairs of the Ways & Means Committees meet as part of the process to develop a state revenue forecast. The current PGSP is 3.6%, which is the same percentage of estimated growth that has always been set in the past. Throughout the years, the healthcare cost benchmark has always defaulted to the PGSP as the basis, including a five year period with a statutory requirement for the benchmark to be set at 0.5% below PGSP.
But according to the U.S. Bureau of Economic Analysis, Massachusetts’ actual GDP growth has averaged 5.0% for the past ten years. In seven of those years, the state GDP growth has exceeded the PGSP amount – and, therefore, also the healthcare cost benchmark. For the past three years, the state’s gross product grew 5.8% in 2023, 7.1% in 2022, and 9.6% in 2021.
MHA has filed legislation this session to base the benchmark on actual historical state economic growth, rather than on the more arbitrary potential state gross product. An Act to Reform the Healthcare Cost Benchmark, sponsored by Rep. Frank Moran (D-Lawrence) and Sen. Mike Moore (D-Millbury) would use the most recent 10-year period to calculate the average growth rate in the state economy that would then be used to inform the HPC’s healthcare cost growth benchmark. Like today, the HPC would still have the ability to recommend a benchmark that is different. Under this approach, however, the benchmark would be initially tied to actual state economic activity as the 2012 law intended.
MHA Budget Letter Lays Out Concerns, Suggestions
Budget season is underway with the filing of the governor’s H.1 proposal and the recent staffing assignments for the legislative committees that will review bills.
Last week, MHA sent an 11-page letter to the leadership of the House and Senate Committees on Ways & Means, outlining the healthcare community’s concerns and suggestions heading into the FY2026 budget process.
The letter acknowledged the difficult fiscal environment the state is facing and the limited availability of funding opportunities. But MHA pointed out that some aspects of the healthcare system demand immediate attention to stop them from evolving into even greater problems for patients, hospitals, health systems, and the state.
First among the concerns is adequate funding of the health safety net, which pays for care services provided to uninsured and underinsured Massachusetts, and which is projected to face a funding shortfall of more than $230 million in the current fiscal year. Hospitals alone are responsible for covering any shortfalls, which have been ballooning in recent years and are expected to worsen in FY2026 unless relief is granted.
While MHA told the legislative leaders it is thankful the governor did not propose any MassHealth rate cuts in her FY2026 budget, such flat funding in the face of rising hospital costs nonetheless equates to a cut in reimbursements. MHA wrote to the Ways & Means leaders that in light of the indirect rate cuts, care should be taken to avoid other cuts and increased administrative burdens associated with MassHealth.
MHA’s budget letter asks, among other initiatives that will be debated in the coming months, for maintaining funding for programs related to behavioral health, and creating a naloxone trust fund to allow hospitals to be reimbursed for distributing the drug directly to patients (they currently aren’t).
Budget season is underway with the filing of the governor’s H.1 proposal and the recent staffing assignments for the legislative committees that will review bills.
Last week, MHA sent an 11-page letter to the leadership of the House and Senate Committees on Ways & Means, outlining the healthcare community’s concerns and suggestions heading into the FY2026 budget process.
The letter acknowledged the difficult fiscal environment the state is facing and the limited availability of funding opportunities. But MHA pointed out that some aspects of the healthcare system demand immediate attention to stop them from evolving into even greater problems for patients, hospitals, health systems, and the state.
First among the concerns is adequate funding of the health safety net, projected to face a funding shortfall of more than $230 million in the current fiscal year. Hospitals alone are responsible for covering any shortfalls, which have been ballooning in recent years and are expected to worsen in FY2026 unless relief is granted. Health Safety Net funding shortfalls are now too large to allocate to hospitals according to existing program rules. The Executive Office of Health and Human Services (EOHHS) is now forced to reduce the minimum amounts the program reimburses Disproportionate Share Hospitals and provide no reimbursement to non-safety net hospitals despite their payments into the fund. MHA requested the legislature consider changes to Health Safety Net financing to address the instability, including revisiting state and insurer contributions to the fund.
While MHA told the legislative leaders it is thankful the governor did not propose any MassHealth rate cuts in her FY2026 budget, such flat funding in the face of rising hospital costs nonetheless equates to a cut in reimbursements. However, MHA raised concern with policy changes that will result in payment reductions to hospitals. MHA wrote to the Ways & Means leaders to reconsider these indirect payment reductions.
MHA’s budget letter asks for, among other initiatives that will be debated in the coming months, maintaining funding for programs related to behavioral health, and creating a naloxone trust fund to allow hospitals to be reimbursed for distributing the drug directly to patients (they currently aren’t).
Court Injunctions on NIH Funding, Gender-Affirming Care
Last Wednesday, a U.S. District Court Judge in Massachusetts granted a nationwide preliminary injunction banning the National Institutes of Health (NIH) from cutting so-called indirect costs, also known as “facilities and administrative” costs, of grants it awards to institutions.
On February 7, Judge Angel Kelley had issued a temporary restraining order to stop the cuts. She held a hearing on that TRO on February 21, and last week issued the preliminary injunction which will be in place until the three lawsuits now challenging the cuts are fully resolved.
The Association of American Medical Colleges, American Association of Colleges of Pharmacy, Association for Schools and Programs of Public Health, and the Greater New York Hospital Association, joined by the Conference of Boston Teaching Hospitals (COBTH) sued the federal government over the NIH decision. Twenty-two Attorneys General, including Massachusetts AG Andrea Joy Campbell also brought suit against the Trump Administration’s unilateral cut of NIH’s facilities & administrative (F&A) costs to universities, medical schools, hospitals, and others engaged in research. A third suit led by the Association of American Universities also challenges the cuts.
F&A costs are those that can’t be tied to a specific research project, but which fund such things as data security and data storage, laboratory equipment, radiation safety, hazardous waste disposal, and more. For example, a health system conducting NIH-funded cancer research receives a sum of money from NIH. Included within that sum to pay researchers’ salaries and costs associated with the specific project are the F&A costs that vary depending on the institution due to differences in wages in the research area for critical research support staff, the type of research and laboratories needed for that research, and other institution-specific reasons. But the NIH announced in February that it would cap such F&A costs at 15%, regardless of the institution, and that announcement triggered the lawsuits. The plaintiffs argued that without full reimbursement of F&A costs to pay for such things as electricity, safety protocols, and maintenance staff, potentially lifesaving research projects would cease.
In her ruling last week, Judge Kelley wrote, “Plaintiffs’ challenge to the lawfulness of NIH’s action and the unique nature of the broad impact of the Rate Change Notice warrants a broad response until final judgment or appellate review, whichever occurs first, resolves the question of the lawfulness of NIH’s actions. Considering the irreparable harm likely to befall similarly situated nonparties, the chaos that would result both for institutions and NIH from a patchwork of injunctions, the diffuse nature of the Plaintiffs, and the nature of the suit, a nationwide preliminary injunction is the appropriate and reasonable remedy.”
“This is a major win for research institutions across the country – in both red and blue states – that rely on NIH funding to conduct innovative research, as well as for the individuals and families who depend on these medical advancements to improve and even save their lives,” said Attorney General Campbell following the ruling.
While health interests applauded the court ruling, they expressed concern over notices that the NIH sent in the days before the court orders were handed down, which rescinded grants to some research projects. The NIH cuts were not related to the grants’ F&A costs but rather were due to the research projects focusing on some element of what the administration considered diversity, equity, and inclusion issues. Court cases around the U.S. are challenging the wholesale denial of funding for existing contracts and it is unclear if the recent NIH cuts are in violation of those court orders.
Last week, federal courts also struck a blow against the president’s executive order that banned federal funding for gender-affirming care for people under age 19. The January 28 executive order, Protecting Children from Chemical and Surgical Mutilation, directed that any agency providing research or educational grants to “medical institutions, including medical schools and hospitals” take immediate steps “to ensure that institutions receiving Federal research or education grants end the chemical and surgical mutilation of children.” And a January 20 order requires all federal agencies to “remove all statements, policies, regulations, forms, communications, or other internal and external messages that promote or otherwise inculcate gender ideology.”
In last Tuesday’s court order granting a nationwide preliminary injunction against the executive orders, Maryland U.S. District Judge Brendan Abell Hurson wrote, “The sudden denial or interruption of plaintiffs’ medical care has caused or is expected to soon cause unwanted physical changes, depression, increased anxiety, heightened gender dysphoria, severe distress, risk of suicide, uncertainty about how to obtain medical care, impediments to maintaining a social life, and fear of discrimination, including hate crimes. Defendants’ assertion-that these injuries are nothing more than ‘hypothetical’ and ‘incidental,’ … is blatantly contradicted by the record.”
The following day, Wednesday, March 5, CMS sent notice to providers stating, “This alert is notice that CMS may begin taking steps in the future to align policy, including CMS-regulated provider requirements and agreements, with the highest-quality medical evidence in the treatment of the nation’s children in order to protect children from harmful, often irreversible mutilation, including sterilization practices.”
And last Thursday, the Health Resources and Services Administration (HRSA) sent a letter to hospitals, citing the CMS notice and adding that it will begin a review of its policies, grants, and programs.
HRSA Administrator Thomas Engels wrote, “HRSA’s review will include its Children’s Hospitals Graduate Medical Education (CHGME) Payment Program. In particular, HRSA will examine the $367.2 million that was awarded in fiscal year 2024 to 59 free-standing children’s hospitals nationwide in light of the concerns discussed in [the CMS memo]. HRSA may also consider re-scoping, delaying, or potentially cancelling new grants in the future depending on the nature of the work and any future policy change(s) HRSA may make.”
In Memoriam: Fletcher “Flash” Wiley
MHA joined more than 1,000 people in Boston last Friday to celebrate the legacy of Fletcher “Flash” Wiley, the civic and business leader who is credited with breaking longstanding barriers for African Americans in the region.
Born into segregation in the Midwest, Wiley served in the U.S. Air Force and moved to Massachusetts in the early 1970s to pursue his law degree. Over the next five decades, he would co-found the largest minority-owned law firm in New England, create and lead a state Commission on Minority Business Development, and serve as the Greater Boston Chamber of Commerce’s first Black chairman. He is remembered for – with joy and humor — pioneering the commonwealth’s efforts to diversify Massachusetts’ executive ranks and economic opportunities, a goal that the state’s healthcare sector has an outsized role in realizing.
Wiley’s son Pratt, while reflecting on his father’s accomplishments, paid special thanks to the local hospitals and the “extraordinary care team” who cared for him in his final years – particularly those at Spaulding Rehabilitation. Pratt Wiley is President & CEO of The Partnership, Inc., and is a member of the MHA Board of Trustees.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association