Advancing Telehealth; Ruling in No Surprises Act

INSIDE THE ISSUE
> Advancing Telehealth
> Insurers Rebuffed in Texas
> Long-Term Care
> State of the Union
> FOCUS ON WORKFORCE: Berkshire Health Systems
> HPC’s Advisory Council
> ACHE of MA Workforce Program
MONDAY REPORT
Preserving Access to Telehealth’s Benefits
Telehealth was a lifesaver for many during the pandemic as it allowed patients to visit their providers virtually, during a time when doctors’ offices and hospitals were crowded with COVID-19 patients.
But since then, despite the proven benefits of telehealth, insurers have been attempting to chip away at what they will cover when patients and providers meet by phone or video conference. The state’s largest commercial insurers have announced they will reduce payment by 20% for chronic care and primary care delivered by telehealth, effective July 1 and March 1, respectively. In the effort to extend telehealth to communities that lack access to affordable broadband or that do not possess “digital literacy,” the fight has been taken up by providers, advocates, and leaders in state government, and not by the health insurance companies.
Now, Rep. Marjorie Decker (D-Cambridge) and Sen. Adam Gomez (D-Springfield) have introduced legislation – HD3511/SD1984, An Act Relative to Telehealth and Digital Equity for Patients – to preserve continued access to telehealth services. Among other things, the bill would require reimbursement parity for all telehealth services to be on par with in-person services by removing existing sunset dates for parity. It establishes task forces to investigate issues surrounding telehealth care for patients who are in other states, including interstate licensure or registration of providers using telehealth. And, importantly, it requires health insurers to participate more fully in helping underserved communities by requiring the insurers to screen for digital health literacy and to offer digital health education to enrollees.
The bill also directs the Health Policy Commission (HPC) to establish two programs—a Digital Bridge Pilot Program and a Digital Health Navigator Tech Literacy Pilot Program—to support expanded access to telehealth technologies and technological literacy. The bill prohibits insurers from imposing prior authorization requirements on medically necessary telehealth visits that would not apply to in-person visits. It further requires insurers to cover interpreter services for patients with limited English proficiency and for those who are deaf or hard of hearing.
The provisions in the legislation follow most of the HPC’s recommendations in a recent report, including extending payment parity for telehealth and continuing payment parity between audio and video visits – a critical equity issue for those who do not have access to broadband services or digital health literacy.
Texas Judge Strikes Down Revised No Surprises Act Dispute Process
On February 6, U.S District Court Judge Jeremy Kernodle ruled in favor of the Texas Medical Association (TMA) in TMA v. U.S. Department of Health and Human Services. The ruling found that HHS’ revised No Surprises Act independent dispute resolution (IDR) process, which determines payments for out-of-network services, was still skewed in favor of commercial insurers.
This ruling continues an ongoing legal dispute over the IDR process between provider groups and the federal government. In 2022, a federal judge struck down part of HHS’ September 2021 interim final rule, which called for IDR arbiters to give the most weight to the IDR submission closest to the qualifying payment amount (QPA), which is the average cost for a service in a geographic area. HHS then released a revised rule in August 2022, aiming to add additional weight to other IDR factors, such as patient acuity and provider training. Despite the revisions, the February 6 ruling found the IDR process to still be lacking the appropriate balance to determine fair reimbursement between commercial insurers and providers.
Last Friday, February 10, CMS said that because of the Texas court ruling, it was ordering all IDR entities to halt all payment determinations and to recall any payment determinations issued after the February 6. The federal government is reviewing the court decision and the current IDR process and will decide on how to proceed in the coming weeks.
The American Hospital Association praised the court ruling, saying that by rejecting the HHS rule, the court “restores the balanced, patient-friendly dispute resolution that Congress chose when it enacted the No Surprises Act. The district court correctly observed that the government’s final rule would have tilted arbitrations in favor of insurers, thereby inappropriately lowering payments to healthcare providers and threatening patient access to care.” AHA, MHA, and other providers nationally have strongly supported federal action to take patients out of the middle of out-of-network billing issues, while advocating for fair payment from insurers.
Need for Short-Term Beds Down; Demand for Long-Term Care Increases
The healthcare system continues to struggle with moving patients efficiently from care setting to care setting, which is causing major backups, capacity constraints, and the misuse of hospital beds.
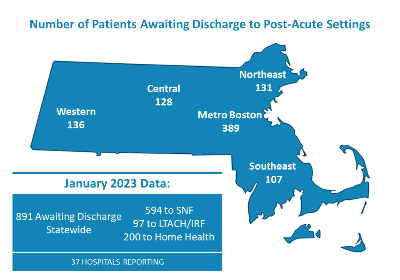
MHA’s monthly “throughput” survey that tracks the number of patients in acute care hospitals that are awaiting discharge to a post-acute setting shows that there was a backup of 891 patients in January. Patients stuck in acute care hospital beds unable to transfer to, say, a rehab hospital or skilled nursing facility, means the hospital bed is unavailable for other patients. That bed is being “misused” because the no-longer-acutely-ill patient occupying it is not receiving care in the most appropriate setting, and an acutely ill patient may be waiting in a hospital emergency department for the bed to become vacant.
One piece of good news in the January MHA report is that it shows some of the lowest demand for short-term rehabilitation beds since the survey began in March 2022. That may be due to the state/healthcare community partnership with nursing facilities to provide dedicated short-term rehabilitation capacity. However, the demand for long-term care beds is at the highest level ever since the survey began. Currently, there are 300 patients statewide who are awaiting placement in a nursing facility’s long-term care bed. More than 250 patients have been waiting more than a month for a post-acute bed; and nearly 50 of those have been waiting more than six months.
Biden in State of the Union: Support for Medicare, Cancer Moonshot
President Joe Biden’s State of the Union speech was laden with healthcare policy ideas. Many are housed within a new “Unity Agenda” that the administration announced before the address, and which targets healthcare-related reforms viewed as ripe for bipartisan support. He highlighted the health provisions included in the Inflation Reduction Act of 2022 and expressed support for extending the $35 cap on insulin to all Americans rather than limiting it to Medicare beneficiaries. Biden also proposed that Affordable Care Act Marketplace premium assistance subsidies be made permanent.
In a tense exchange with Republicans during the address, the president expressed his support for the Medicare program, saying that he will oppose any cuts to its funding. He also discussed Administration efforts to increase nursing home oversight and address the behavioral health crisis. Finally, Biden highlighted the “Cancer Moonshot” project and several initiatives related to it. A fact sheet detailing key healthcare priorities is here.
FOCUS ON WORKFORCE:
BHS Grows its Workforce Through Talent Pipeline Program

In a decisive move to address staffing challenges and continue to build a skilled healthcare workforce in the Berkshires, that county’s largest employer, Berkshire Health Systems (BHS), has launched a series of workforce development pipeline programs that are opening new career paths for hundreds of nursing assistants, medical assistants, licensed practical nurses, and registered nurses.
BHS is experiencing the same staff vacancy and high-turnover-rate challenges being felt across Massachusetts and the U.S., but is taking action to turn the tide, investing significant resources – about $7 million – in developing career pipeline programs in high-need clinical areas.
One area of significant pipeline growth has been in the Nursing Assistant Training Program, which helps train and place candidates as nursing assistants at Berkshire Medical Center. Program participants receive three weeks of intensive, on-the-job training from an expert team of nurse educators and are eligible to receive full-time nursing assistant wages and benefits as soon as they begin their training. At the conclusion of their training, nursing assistants are accepted into full-time caregiving positions at the hospital.
“The students participating in the Nursing Assistant Training Program are learning this is a unique way to build a path to a rewarding career, give back to their community, and experience a real sense of pride in what they can accomplish,” said Betty Kirby, BHS Director of Education.
Read the rest of the story about Berkshire Health System’s workforce strategy, as well as workplace stories from other providers throughout the state, by visiting MHA’s Workforce Toolkit.
HPC Advisory Council’s New Members
The Health Policy Commission Advisory Council – a 34-member group that advises the HPC staff and its commissioners – met for the first time in its 2023-24 term last week. The Council has 10 new members, including the following from MHA’s membership: Aimee Brewer, president and CEO, Sturdy Memorial Hospital; Dr. Jeanette Callahan, pediatrician, Cambridge Health Alliance, and medical director, Department of Youth Services Northeast Region Health Services, Justice Resource Institute; Susan Hernandez, Mass General Brigham, MA American College of Nurse-Midwives, legislative co-chair; Juan Fernando Lopera, chief diversity, equity, and inclusion officer, Beth Israel Lahey Health; and Patricia “Tish” McMullin, executive director, Conference of Boston Teaching Hospitals. Emerson Health President & CEO and MHA Board of Trustees Chair Christine Schuster, R.N., and MHA President & CEO Steve Walsh also serve on the Advisory Council.
During the term’s kickoff meeting, the Advisory Council reviewed the HPC’s “Agenda for Action” for the first six months of the year. A priority of the agenda is to address the current healthcare workforce crisis. HPC said that in the next six months it plans to issue a report and recommendations on the topic, hold a special event to convene stakeholders to discuss workforce challenges and recommended solutions, and continue to promote innovative care models that “leverage non-traditional and complementary healthcare workers (e.g., doulas, recovery coaches, community health workers).”
ACHE to Hold Special Workforce Program
ACHE of Massachusetts is holding a virtual program entitled Staying Nimble Through the Healthcare Staffing Crisis on Tuesday, February 28 from 5 to 6:30 p.m. The program will look at the staffing challenges through the lens of creative strategies, such as shifting working hours in various ways, creating new types of workers/roles within systems, improving the educational pipeline, and employing technology solutions. The program will address the question: with the high cost of living in Massachusetts, how can healthcare organizations attract and retain talent to propel their organizations through a challenging time while building a strong talent pipeline?
Panelists include MHA’s Vice President of Clinical Affairs Patricia Noga, R.N., PhD; Kyle Deskus, associate general counsel, Baystate Health; Guy Evans, president Symmetry Workforce Solutions, Aya Healthcare; and Therese Fitzpatrick, PhD., R.N., senior vice president, Kaufman Hall. Credits are available. Click here for more information and to register.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association