INSIDE THE ISSUE
> Patients Awaiting Discharge
> Pending Legislation
> Drug Deaths
> Equity
> Baby Formula
MONDAY REPORT
1,000+ Patients Awaiting Discharge to Post-Acute Settings
At any given time, there are approximately 1,000 patients in Massachusetts acute care hospitals who are ready to be discharged but are stuck awaiting the next level of care.
Delays in patient discharges to post-acute care settings have become a growing challenge for hospitals and post-acute care providers. While such issues were significant before the pandemic, COVID-19 exacerbated the situation and created a large volume of patients who are ready for discharge from hospitals but cannot find an appropriate bed in a post-acute care setting. In some cases, patients who require specialized post-acute care services wait weeks or even months to find an appropriate bed or service.
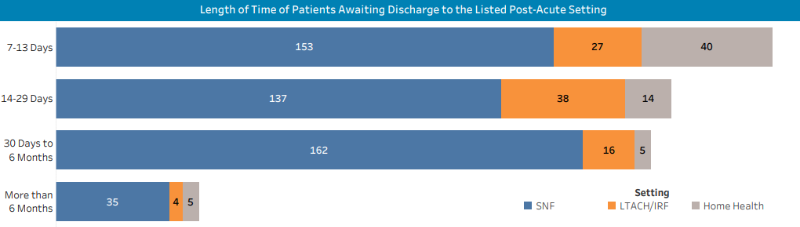
The most recent survey of hospitals from MHA, in partnership with members of the post-acute sector, shows that at a point of time in May 2022, forty-four hospitals reported that 1,022 patients had been waiting between one and six months to be discharged to a skilled nursing facility (SNF), a long-term acute care hospital (LTACH), inpatient rehabilitation facility (IRF), or a home health agency. An additional 44 patients had been waiting more than 6 months for discharge to one of those facilities.
These patients are distinct and separate from the weekly 600 to 700 behavioral health patients that each week board in hospital emergency departments and units awaiting a psychiatric inpatient bed (see story below).
The survey showed 672 of the total patients were awaiting discharge to SNF, 105 to LTACH/IRF, and 289 to home health. Taken in whole, the results show yet another layer of pressures healthcare organizations, and the patients in their care, are currently experiencing.
According to the MHA report, the reasons for the discharge delays of the stuck patients are numerous. The most dominant obstacle cited among respondents involves private insurance administrative barriers, including delayed responses or denials of authorization requests. Another major contributing factor to the “throughput” problem is that skilled nursing facilities, and other post-acute providers, are facing staffing shortages, meaning that while a bed may be available, the workers to staff them are in short supply.
Early in the pandemic, MHA stood up a Post-Acute Transitions of Care & Emergency Preparedness Workgroup with partners in the post-acute care ecosystem to address patient transition challenges and capacity constraints for hospitals and post-acute care services. MHA also partnered with the Massachusetts Senior Care Association to establish a Post-Acute Care Transition Collaborative to support hospital discharge case managers and escalate and address challenges in skilled nursing facility placements. The Baker Administration has also partnered with MHA and Mass. Senior Care to create a temporary program that has helped by adding short-term rehabilitation capacity in all regions of Massachusetts; however, the sheer volume of patients who need post-acute care has continued unabated.
MHA’s new Throughput Survey will be continued on a monthly basis and is intended to inform both short-term policy development and longer- term solutions to best ensure all patients have access to needed services in a timely manner.
Session Drawing to Close; Key Bills Pending
The Massachusetts legislature has moved into high gear as the session draws to a close on July 31. In addition to the House-Senate conference committee that has begun to meet over the FY2023 state budget, other bills are of great interest to the healthcare community are rumored to be inching to completion.
MHA considers the workplace violence prevention legislation that is expected to move out of committee this week to be the most impactful bill of the session. Ensuring that it is comprehensive in its reach and the standards for risk assessment at facilities are outlined clearly, among other factors, will determine if the bill succeeds in its goals, MHA has told legislative leaders.
“The work to improve safety never ends, and hospitals are well positioned to evolve their protocols and practices based on the world around them,” said Steve Walsh, MHA’s president & CEO.
Another bill – one that reflects an idea that has been discussed for years – involves the state joining 38 other states that are part of the national Nurse Licensure Compact (NLC). The NLC allows nurses to have one multistate license from the state in which they reside, with the privilege to practice in their home state and all others that are members of the Compact. Nurses must go through stringent licensing requirements – including criminal background checks – to join the Compact. In non-Compact states such as Massachusetts, licensed nurses from out of state wishing to practice in the commonwealth must go through a lengthy, resource-intensive review by the state licensing board. Hospitals report that a lengthy state review often results in a nurse who is offered a job in Massachusetts ultimately choosing to immediately practice elsewhere as opposed to waiting for the Massachusetts approval. Another benefit of Massachusetts joining the NLC is that it will allow Massachusetts-based nurses “to follow” their patients by telemedicine over state lines into other Compact states.
Governor Baker supports the NLC as do many legislative leaders, as well as healthcare groups such as the Organization of Nurse Leaders and American Nurses Association Massachusetts. In May 2021, the state’s Health Policy Commission (HPC) voted to recommend that Massachusetts join the Compact, finding, among other benefits, that NLC membership would help Massachusetts “react more dynamically to unforeseen and sudden changes in nursing needs, during pandemics and other emergencies.” In a 2014 survey of Massachusetts nurses, two-thirds of respondents expressed support for entering the Compact.
MHA expressed hope last week that the logjam on the NLC will be broken in the coming weeks and that legislators send the bill to the governor.
Drug Death Total Worsened in 2021
Opioid-related deaths in Massachusetts during all of 2021 increased by 8.8% over the previous year – for a total of 2,290 lost lives, according to the most recent Department of Public Health report. It is the highest number of drug-related deaths recorded in the state. According to the federal Centers for Disease Control and Prevention, 107,622 Americans died of drug overdose in 2021 – a 15% increase over the previous year.
According to the DPH report, “In 2021 there were 2,119 opioid-related overdose deaths where a toxicology screen was also available. Among these deaths, fentanyl was present in 93%, cocaine in 51%, benzodiazepines in 31%, alcohol in 29%, prescription opioids in 13%, heroin in 10%, and amphetamines in 10%.” DPH said much of the fentanyl occurring in Massachusetts is an illicitly produced product, and not diverted pharmaceutical fentanyl.
MHA’s point person on the substance use disorder issue, Leigh Simons Youmans, MHA’s senior director, healthcare policy, said MHA’s members are reporting that the pandemic “fast-tracked many of the stressors and environmental factors that often lead to substance use disorder – especially among people of color.” She added that MHA is “grateful for the attention and resources that the state is devoting to address this crisis. MHA and our members remain firmly committed to being a leader in this fight, using the same sense of urgency and community connections that have gotten us through the pandemic. We are asking people to use this news as a call to action: please check in with those in your lives who are trying to overcome addiction and help them find the resources they need.”
Spreading the Equity Message
MHA’s Director of Health Equity Akriti Bhambi is scheduled to address the legislature’s Women’s Caucus tomorrow to discuss the healthcare community’s role in addressing the social determinants of health, and expanding access to dependable, affordable, and equitable care, among other topics. MHA and the healthcare community have redoubled their efforts to include diversity, health equity, and inclusion (DHE&I) in their operations. MHA has created a board-level Standing Committee on Diversity, Health Equity, & Inclusion and holds frequent education programs on DHE&I issues, among other actions. MHA, its membership, and the state are also currently engaged in the seeking federal approval for the state’s five-year Medicaid waiver proposal, which contains an innovative mechanism for tying Medicaid payments to health equity improvements across the state.
Baby Formula Crisis Seems to Be Easing
In a conference call last week with hospital and healthcare interests, Food and Drug Administration Commissioner Robert Califf reported that the national shortage of baby formula is easing. Ever since a February voluntary recall of formula from the nation’s largest producer – Abbott Nutrition in Michigan – regular infant formula (sold as Similac) and specialty formulas have been in short supply. Califf said the Michigan plant in producing again and imports are up.
Any hospital needing either normal formula or specialty formula should contact Abbott Nutrition directly. The FDA says it has cleared the release of a large amount of specialty formula previously held in the Sturgis plant and there is ample inventory available.

 Massachusetts Health & Hospital Association
Massachusetts Health & Hospital Association 